Social Security Disability Benefits Guide for Veterans
Some veterans receiving VA disability benefits may qualify for Social Security disability as well. These are two separate benefits, awarded through the Department of Veterans Affairs and Social Security Administration respectively, so veterans will need to apply for each separately.
The main difference between veterans disability and Social Security disability is that the VA grants benefits based on varying degrees of disability, while the SSA makes a determination as to whether a claimant is disabled or not. You either receive full Social Security benefits or not.
It’s also important to note that your VA disability compensation will count as income and potentially lower your Social Security payments.
The attorneys at Hill & Ponton put together this guide for veterans seeking social security disability benefits in addition to their VA benefits.
- Which Social Security Disability Benefits Can Veterans Receive?
- How Does The Social Security Administration Determine Disability for Veterans?
- How Do Veterans Apply for Social Security Disability?
- What Evidence Do You Need for Your Application?
- Filing Your Social Security Claim: Tips for Veterans
- 5 Secrets to Winning Your Disability Claim
- 7 Mistakes to Avoid When Filing for Social Security Disability Benefits
- Tools to Help with Your VA Claims
Which Social Security Disability Benefits Can Veterans Receive?

Veterans may be eligible for two types of Social Security benefits: Supplemental Security Income (SSI) or Social Security Disability Insurance (SSDI). The SSA expedites applications for veterans who became disabled during active military service on or after October 1, 2001, as well as veterans with 100% permanent and total disability status.
The Social Security Administration doesn’t take your VA approval into account when determining your eligibility for Social Security disability. While there was a time when a high VA rating helped your changes of SSA approval, the SSA changed this in 2017. The SSA will also not consider your discharge status or whether your disability is connected to military service.
Supplemental Security Income (SSI)
SSI benefits provide income to individuals who are disabled, blind, or over age 65 and demonstrate financial need. In other words, SSI is income based. There are very restrictive limitations on what assets you can have and what income you can make and receive these benefits.
When applying for SSI, veterans should keep in mind that their VA disability compensation counts as income and will lower their SSI payments.
Social Security Disability Insurance (SSDI)
If you have worked and paid enough Social Security taxes, and you are disabled, you may be entitled to SSDI benefits. These benefits are also called Disability Insurance Benefits (DIB). The total payment you receive will generally depend on what you have paid into the system through social security withholding taxes.
Your VA disability payments will have no effect on your eligibility for SSDI.
Medicare
The SSA automatically awards Medicare coverage once you’ve received your disability benefits for 24 months.
How Does The Social Security Administration Determine Disability for Veterans?

Veterans applying for Social Security disability benefits need to meet several eligibility criteria.
To be eligible, you:
- Must be unable to do substantial work because of your medical condition(s); AND
- Your medical condition(s) must have lasted, or be expected to last, at least one year or result in death.
Again, while the VA awards disability benefits for partial or short-term disability, the SSA does not. Veterans need to fully meet these requirements to be eligible.
In some cases, an applicant’s condition will improve, and the SSA would no longer deem them disabled. In this case, the veteran would qualify for a “closed period of disability.” The requirements include:
- Medical evidence must show that the applicant was “unable to engage in substantial work for a continuous period of 12 months,” but the applicant’s condition improved by the time the disability decision was made.
- The applicant must file an application within 14 months after the disability ended.
- Applicants that meet the above requirements must wait five months before their first disability payment. Applicants can receive up to 12 months of retroactive benefits from the filing date.
What Does SSA Consider Substantial Work?
When processing SSI and SSDI applications, SSA considers whether you’re able to engage in substantially gainful activity (SGA). The SGA threshold for 2021 is $1,310 per month. If you earn over this amount, you’re participating in substantial work and won’t be eligible.
How Do Veterans Apply for Social Security Disability?
There are a few ways to apply for Social Security benefits:
- Apply through the online application.
- Visit or call your local Social Security office.
- Call the SSA at 1-800-772-1213 (TTY 1-800-325-0778 if you are deaf or hard of hearing).
If you’re eligible for expedited processing, the SSA will automatically determine this.
What Evidence Do You Need for Your Application?
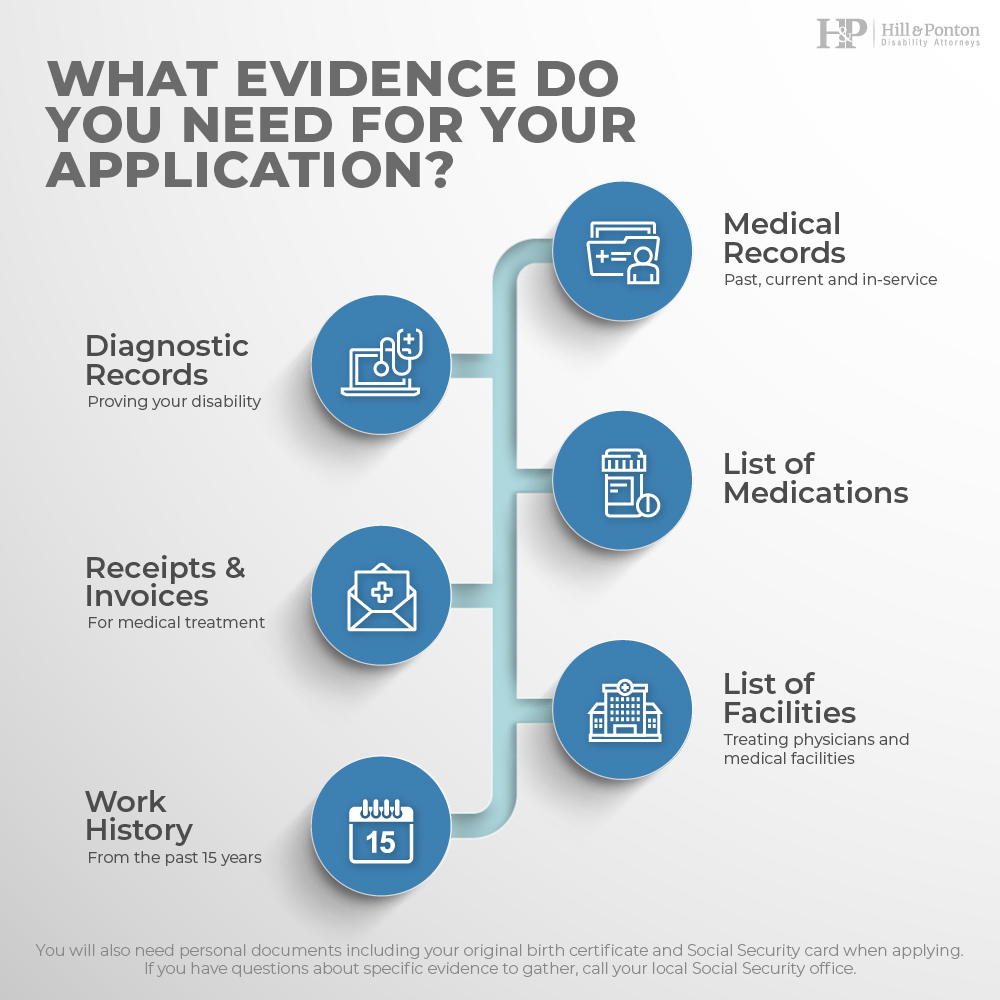
The evidence you gather for your SSI and SSDI applications are similar to that for your VA disability claim.
Be sure to have evidence, including:
- Medical records (past, current, and in-service)
- Diagnostic records proving your disability
- List of medications
- Receipts/invoices for medical treatment
- List of treating physicians and medical facilities
- Work history from the past 15 years
You will also need personal documents including your original birth certificate and Social Security card when applying. If you have questions about specific evidence to gather, call your local Social Security office.
Filing Your Social Security Claim: Tips for Veterans
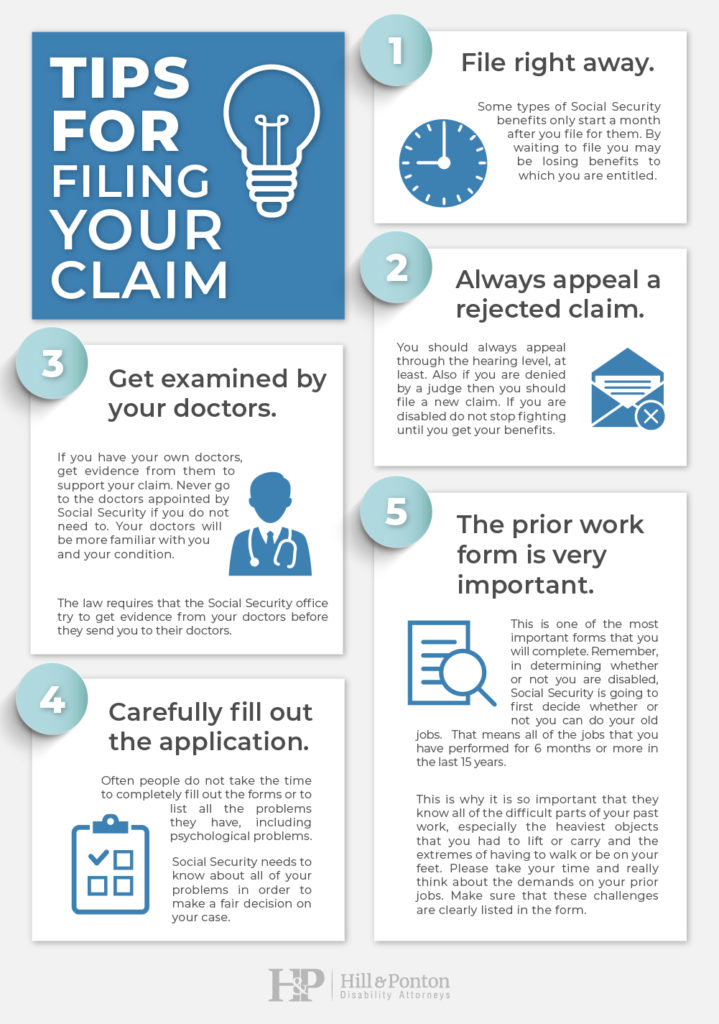
As you fill out your Social Security disability application, there are a few best practices to keep in mind.
1. File right away.
Some types of Social Security benefits only start a month after you file for them. By waiting to file you may be losing benefits to which you are entitled.
2. Always appeal a rejected claim.
You should always appeal through the hearing level, at least. Also if you are denied by a judge then you should file a new claim. If you are disabled do not stop fighting until you get your benefits.
3. Be sure to get examined by your doctors.
If you have your own doctors, get evidence from them to support your claim. Never go to the doctors appointed by Social Security if you do not need to. Your doctors will be more familiar with you and your condition.
The law requires that the Social Security office try to get evidence from your doctors before they send you to their doctors.
4. Fill out the application carefully.
Often people do not take the time to completely fill out the forms or to list all the problems they have, including psychological problems. Social Security needs to know about all of your problems in order to make a fair decision on your case.
5. The prior work form is very important.
This is one of the most important forms that you will complete. Remember, in determining whether or not you are disabled, Social Security is going to first decide whether or not you can do your old jobs. That means all of the jobs that you have performed for 6 months or more in the last 15 years.
This is why it is so important that they know all of the difficult parts of your past work, especially the heaviest objects that you had to lift or carry and the extremes of having to walk or be on your feet. Please take your time and really think about the demands on your prior jobs. Make sure that these challenges are clearly listed in the form
5 Secrets to Winning Your Disability Claim
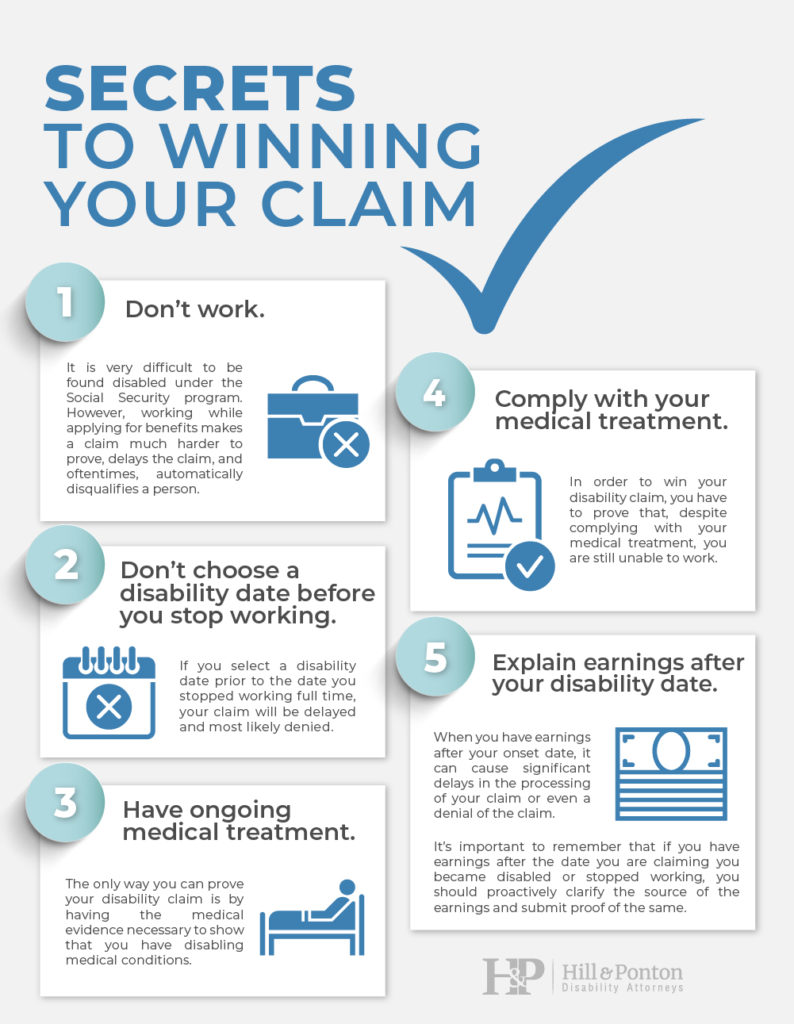
As with VA disability benefits, obtaining Social Security disability isn’t always easy. Here are some tips for a successful outcome.
1. Don’t work.
It is very difficult to be found disabled under the Social Security program. However, working while applying for benefits makes a claim much harder to prove, delays the claim, and oftentimes, automatically disqualifies a person.
The only exception made for a working disabled individual is if the person is legally blind. They have their own set of complicated rules and regulations. However, for all others, if you are making approximately $1,310 (2021) a month or more, you are automatically disqualified from receiving benefits.
Your claim won’t even be reviewed medically because technically, you cannot qualify. In addition, if you make less than $1,310 (2021) a month, though your application will be taken, your chances of being approved significantly decreases and your processing time increases.
If you stop working after you have applied or if you attempt to work after you have applied, means more work for the Social Security representative which causes added delays in the processing of your claim.
2. Don’t choose a disability date before you stop working.
Selecting your “onset date of disability” is a key factor in proving your disability claim. Multiple factors need to be considered when selecting a date and one that can be proven. This is not a cut and dry decision. However, what is true in most cases is that if you select a disability date prior to the date you stopped working full time, your claim will be delayed and most likely denied
3. Make sure you have ongoing medical treatment.
We know that having ongoing medical treatment may be easier said than done when you are out of work and uninsured. However, the only way you can prove your disability claim is by having the medical evidence necessary to show that you have disabling medical conditions. You also need to show that these conditions are severe enough to require ongoing medical treatment and cause ongoing limitations that prevent you from working.
In most cases Social Security will not accept your financial hardship as a reasonable explanation for lack of treatment. Rather, the general thinking is that if you really need treatment, you will find a way to get it, whether through a county clinic or program, by borrowing money, or setting up a payment plan to get the treatment you need. The bottom line is that ongoing medical treatment will be critical to proving your disability claim.
4. Comply with your medical treatment.
In correlation with the above tip, it is as important to comply with your physician’s prescribed medical treatment than it is to have it. In order to win your disability claim, you have to prove that, despite complying with your medical treatment, you are still unable to work.
The point is: are you doing all you can to comply with your doctor’s prescribed course of treatment?
And despite your compliance, are you still unable to work?
If you disagree with your physician’s recommended treatment plan, then you should discuss this with your physician. They can then document this and explore potential treatment alternatives.
5. Explain any earnings after your disability date.
Your date of disability, known as your “onset date”, is the date you are claiming that your disability began. When you have earnings after this date, it can cause a significant delay in the processing of your claim. And in many cases, these earnings can cause your claim to be denied. Earnings do not always result from working. They can also result from other sources such as:
- Paid Sick Time
- Paid Vacation Time
- Short Term Disability
- Long Term Disability
- Owed Commissions
It’s important to remember that if you have earnings after the date you are claiming you became disabled or stopped working, you should proactively clarify the source of the earnings and submit proof of the same.
7 Mistakes to Avoid When Filing for Social Security Disability Benefits
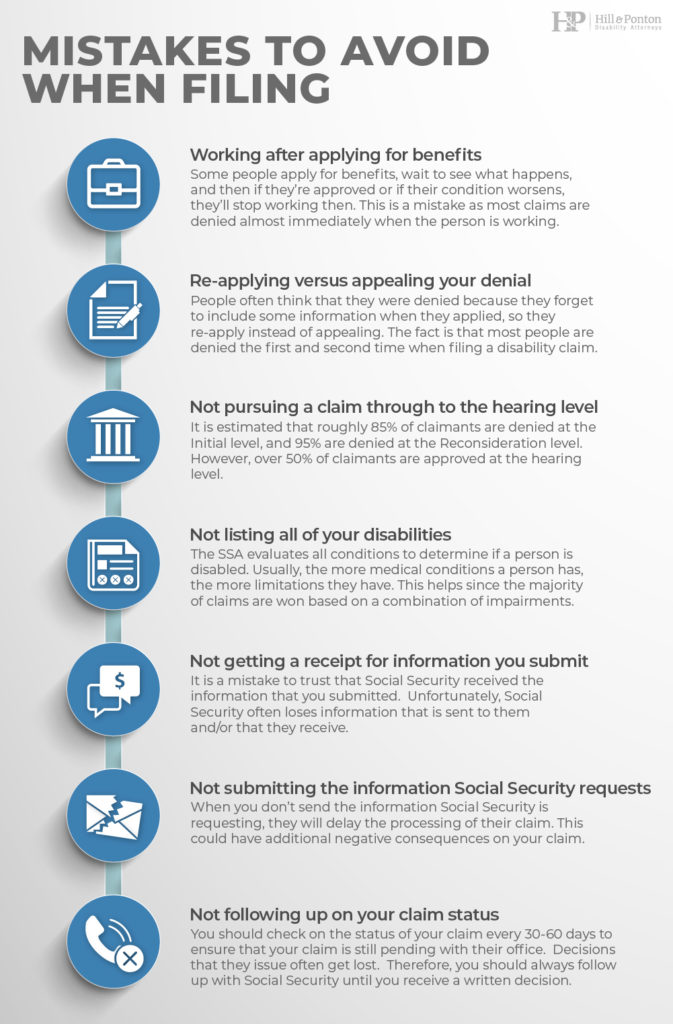
1. Working after applying for benefits
Sometimes people think that they can apply for benefits, wait to see what happens, and then if they’re approved or if their condition worsens, they’ll stop working then. This is a mistake, since most claims are denied almost immediately when the person is working and making over $1,310 (2021) a month.
2. Re-applying versus appealing your denial
Many times, when claimants apply and are denied, they will let their appeal time lapse and will file a new application instead. This is a serious mistake.
People often think that they were denied because they forget to include some important information when they applied, so they will decide to re-apply instead of appealing their existing denial. The truth is that most people are denied the first and second time when processing a disability claim.
There are also long waiting periods at each and every level. Therefore, it is much more beneficial to appeal Social Security’s decision and include the additional information in the appeal. This way, you won’t lose the time you already spent waiting on Social Security’s first decision, and you will keep your case moving forward.
3. Not pursuing a claim through to the hearing level
Most claims are denied at the Initial and Reconsideration levels. This happens to even severely-disabled individuals. The hope is that the disabled person will be discouraged by the denial and not pursue their claim.
Not pursuing the claim is a huge mistake, especially since the majority of approved claims are approved at the hearing level. It is estimated that roughly 85% of claimants are denied at the Initial level, and 95% are denied at the Reconsideration level. However, over 50% of claimants are approved at the hearing level.
4. Not listing all of your disabilities
Often, a disabled individual will want to claim disability benefits for “a disability”. They will even become angry when Social Security asks about other conditions that they feel are unrelated to their claim. They might ask, “Why is Social Security asking me about my depression when I’m claiming disability due to my heart condition?’.
When evaluating a disability claim, the SSA evaluates all conditions to determine if a person is disabled. Usually, the more medical conditions a person has, the more limitations they have. This helps their case since the majority of claims are won based on a combination of impairments.
Remember, the SSA’s process is different from the VA’s. They determine whether you’re disabled or not, rather than awarding benefits for varying degrees of disability. So, you want to list all possible disabilities to support your claim.
5. Not getting a receipt for information you submit to Social Security
It is a mistake to trust that Social Security received the information that you submitted. Unfortunately, Social Security often loses information that is sent to them and/or that they receive. We recommend that all correspondence mailed to Social Security be sent via certified mail with a signed return receipt requested. If you submit information online, get an electronic receipt, and keep your fax confirmation if you fax any materials.
6. Not submitting the information Social Security requests
Most claimants hate the tedious forms Social Security and the Office of Disability sends them to complete. Oftentimes, the same forms are sent at the second level of a claim as the first. Claimants won’t complete these forms because they feel they have already answered the questions.
This is a mistake. When you don’t send the information Social Security is requesting, they will delay the processing of their claim. This could have additional negative consequences on your claim.
7. Not following up on your claim status
First, you should follow up to make sure that Social Security received all of the information you submitted. Second, you should confirm that the information they received included all of the information they wanted and that they are not waiting for any additional information you need to supply.
Once this is done, you should then check on the status of your claim every 30-60 days to ensure that your claim is still pending with their office. Decisions that they issue often get lost. Therefore, you should always follow up with Social Security until you receive a written decision.
Applying for both Social Security and VA disability benefits is no easy feat. However, by taking the time to do so, you’re ensuring that you receive all of the support you’re entitled to as a veteran.