Coronary Artery Disease (CAD) is a common condition among veterans, particularly those exposed to Agent Orange during their service. The coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to plaque buildup, leading to chest pain, heart attacks, and other serious heart issues.
The VA recognizes the significant impact of CAD on veterans’ health and offers disability ratings to provide necessary compensation.
How Does the VA Rate CAD?
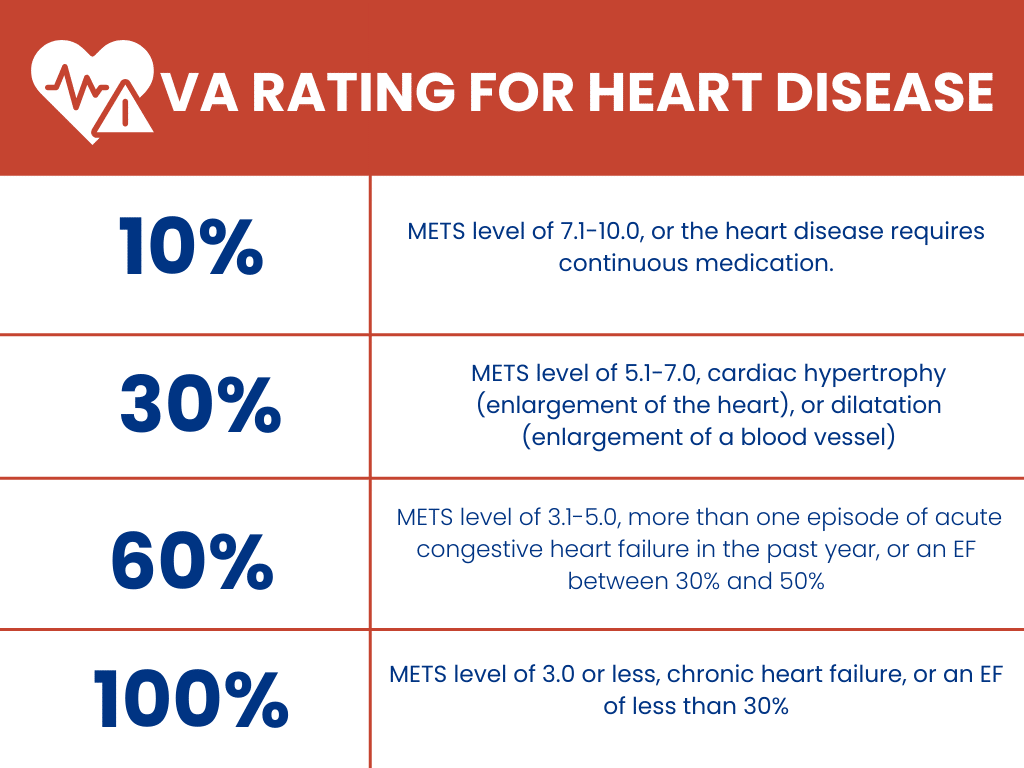
The VA rates CAD based on the severity of the condition and its impact on the veteran’s ability to work and perform daily activities. Ratings range from 10% to 100%, reflecting the extent of the disability and corresponding compensation levels.
Conditions that Fall Under the Coronary Artery Disease Umbrella
Several conditions are categorized similarly to CAD, including:
- Angina (chest pain)
- Myocardial infarction (heart attack)
- Atherosclerosis (plaque buildup in the arteries)
- Chronic ischemic heart disease
These conditions are interconnected and can significantly affect a veteran’s health and quality of life, warranting varying levels of VA disability compensation.
Is CAD a Presumptive Condition?
Agent Orange, a herbicide used during the Vietnam War, has been linked to numerous health issues, including CAD and other heart conditions. Veterans exposed to Agent Orange are at higher risk for developing them, and the VA recognizes this connection by offering presumptive service connection for ischemic heart disease, which includes CAD.
This means eligible veterans will receive VA disability compensation without needing to prove a direct service connection. For those exposed to Agent Orange, the presumption of service connection simplifies the path to obtaining deserved benefits for CAD and related conditions.
Successful Increase of Noncompensable (0%) Rating
Claim File Referenced Here
A veteran initially received a noncompensable (0%) rating for coronary artery disease with arteriosclerosis. However, after presenting new medical evidence that demonstrated the true severity of his condition, the veteran successfully secured a 60% disability rating.
Ejection Fraction Findings: On October 19, 2010, a VA echocardiogram revealed that the veteran had an ejection fraction of 45 +/- 5 percent. This crucial finding aligned with the criteria for a 60% disability rating under the VA’s diagnostic code for coronary artery disease, which requires an ejection fraction between 30% and 50%.
2004 CT Scan: The veteran’s post-service medical records initially only showed generalized arteriosclerosis, but no direct evidence of coronary artery disease. This was reflected in an August 2004 VA CT scan, which detected calcification of the aorta without indicating a specific heart condition.
December 2010 Nuclear Radiology Consultation: The veteran’s MET level was measured at 4.8 METs, further supporting the case for a higher rating due to the physical limitations caused by his heart condition.
January 2012 VA Heart Examination: The veteran underwent a VA heart examination in January 2012, where his METs level was assessed at >3-5, consistent with activities such as light yard work or brisk walking. This examination confirmed ongoing symptoms of dyspnea, dizziness, fatigue, and occasional syncope, which were vital in maintaining the 60% rating.
Ultimately, the Board of Veterans’ Appeals recognized the veteran’s worsening condition and granted a 60% disability rating effective from October 19, 2010. This case highlights the importance of thorough medical evaluation and the role of specific diagnostic tests, such as ejection fraction measurements, in securing a higher VA disability rating.