Many Veterans experience sleep disorders that may be attributable to either their military experiences or secondary to another condition that may be service-connectable. In this blog, we will explore various types of sleep disorders and what conditions they may be linked to.
Whenever you have disability service-connected by the VA, you should immediately see what conditions are secondary to the service-connected one. For example, a Veteran is service-connected for Diabetes Type II. If that Veteran also has Diabetic Neuropathy, that is a condition that can be claimed as a secondary condition to the Diabetes.
There are several different types of sleep disorders that can be rated for disability by the VA. They fit into 6 different types of sleep disorders:
- Insomnia
- Sleep Related Breathing Disorders
- Hypersomnolence
- Circadian Rhythm Sleep-Wake Disorders
- Parasomnias
- Sleep related Movement Disorders
Sleep disorders are diagnosed using criteria from the International Classification of Sleep Disorders (ICDS), which was created to differentiate between disorders and facilitate an understanding of symptoms, etiology, and pathophysiology that allows for proper treatment. There are six identified ICDS-3 Sleep Disorder categories. A polysomnograph, or sleep study, can accurately diagnose sleep disorders and your doctor can request a study be done if you are experiencing sleep problems.
We will look at each type of disorder, the potential causes or links to other conditions, and what evidence you will need to file a claim for the disorder. Remember, for any claim, you must have an actual diagnosis, with one exception; if you are a Gulf War Veteran, Gulf War Syndrome included undiagnosed sleep related conditions.
Insomnia
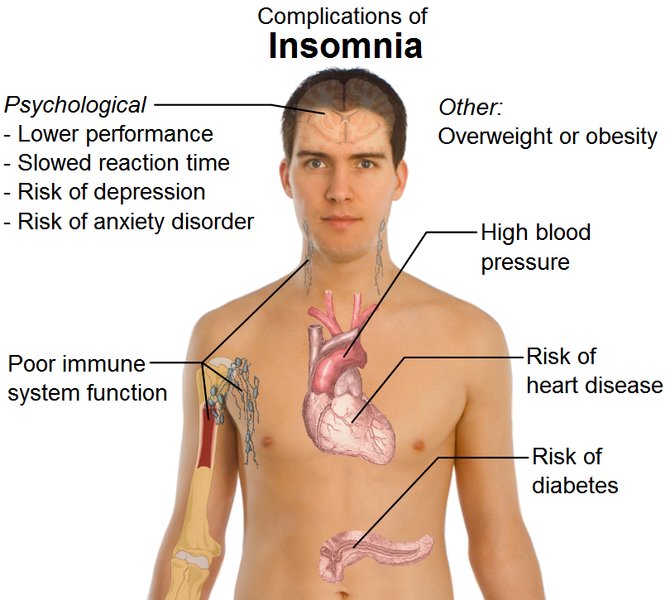
Insomnia is usually claimed as a secondary disability due to being the result of a medical condition that is service connected. Insomnia can be secondary to such disorders as arthritis, gastrointestinal problems, asthma and other respiratory problems, conditions that result in chronic pain, and neurological conditions such as Parkinson’s disease. Insomnia can also be a secondary condition related to medications being taken for a service connected disability such as high blood pressure, heart disease, thyroid disease, depression, and asthma.
Sleep Related Breathing Disorders
Sleep related breathing disorders include such conditions as Obstructive Sleep Apnea, Central Sleep Apnea, and snoring. Not all of these are recognized by the VA as a service connectable disability, and even those that are, it must be shown that it is “as likely as not” related to an event, illness, or injury sustained in service for the disorder to be service connected.
Obstructive Sleep Apnea (OSA) is the most common of the breathing disorders to be service connected. OSA is often related to exposures such as burn pits, oil fires, sand/dust, and pollutants from the Gulf War era. Despite popular belief, OSA is not presumptive for Gulf War Vets; “Undiagnosed Sleep Disorders” is presumptive but difficult to prove. For OSA however, there are specific criteria to get rated; there must be a functional impact and daytime complications. This can include fatigue, lack of concentration, memory problems, high blood pressure, Type 2 Diabetes, liver problems, and even heart conditions.
While OSA is often secondary to respiratory issues such as chronic bronchitis or COPD, often due to the exposures mentioned above which can be service connected. OSA can also be secondary to several medications that are sedatives due to relaxing the muscles of the throat during sleep.
Hypersomnolence
This disorder relates to conditions that cause excessive daytime sleepiness such as narcolepsy, insufficient sleep syndrome (which is different than insomnia), and hypersomnia due to a medical disorder, medication, or psychiatric disorder. Most hypersomnolence conditions are not considered service connectable disabilities with the exception of those secondary to a medical disorder, medication, or psychiatric disorder. Service connected medical disorders associated with hypersomnolence would include such conditions as brain injury, autoimmune disorders, and exposure to environmental toxins such as heavy metals, pesticides, and smoke.
 Circadian Rhythm Sleep-Wake Disorders
Circadian Rhythm Sleep-Wake Disorders
Sleep-wake disorders include such conditions as jet lag, shift work disorder, and non-24-hour sleep-wake rhythm disorder. Most of these are environmental and/or do not cause enough impairment that the VA recognizes them as a disability.
Parasomnias
Parasomnias are REM disorders such as nightmare disorders and REM sleep behavior disorder; NREM parasomnias such as night terrors and sleepwalking; and other parasomnias such as sleep related hallucinations and teeth grinding. This classification would usually be found as symptoms rather than secondary conditions. These types of conditions are usually found as symptoms to PTSD. They can also be triggered by OSA, certain medications, and traumatic brain injury. Again, these are usually symptoms rather than separate conditions and therefore would not be rated separately.
Sleep Related Movement Disorders
This classification of conditions includes Restless Leg Syndrome or Periodic Limb Movement Syndrome, and sleep related leg cramps. Restless Leg Syndrome (RLS) is the most common and is usually a result of a chronic disease or medications such as antidepressants and allergy medications.
Sleep Disorders secondary to Psychiatric Conditions
Some sleep disorders are commonly found related to PTSD and other psychiatric conditions. They are, however, common symptoms of psychiatric conditions and not able to be rated separately from a mental health rating. This is specifically true to Obstructive Sleep Apnea and PTSD. However, if you have filed a rating for a sleep disorder and it has not been finalized; meaning that you have kept the claim open with appeals or the submission of evidence; and have filed a separate claim for PTSD later, that PTSD claim may be able to go back to the original sleep disorder claim. This is something an attorney would be able to determine for you based on the evidence in your Claims File. It does not cost anything to have one of our attorneys review the case.