Chronic inflammatory demyelinating polyneuropathy (CIDP) is a neurological disorder characterized by gradually increasing sensory loss and weakness associated with the loss of deep tendon reflex in the legs and arms. The hallmark of a peripheral nerve disease is loss of ankle reflex. This is when your doctor hits your Achilles tendon and there is no reflex.
CIDP is a progressive motor and sensory neuropathy that is very painful and debilitating. CIDP is caused by damage to the covering of the nerves, called myelin.
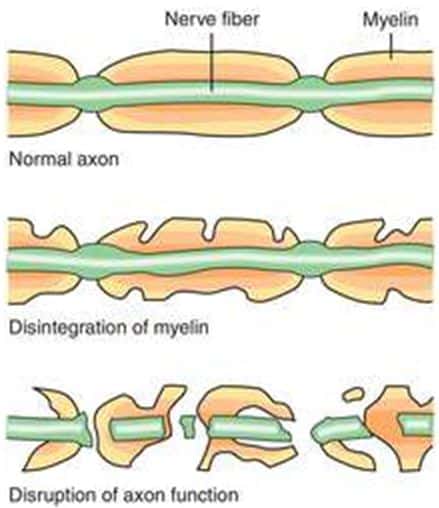
The axon (nerve fiber) works like an electric wire. The myelin sheath around the axon is the insulation necessary for the nerve to conduct electrical impulses properly. In CIDP, myelin is attacked through very complex mechanisms. In such cases, the body sees the peripheral nerve as foreign and antibodies bind to the myelin and begin to break it down. In people with CIDP, this translates into symptoms. For example, if you want to move your finger, messages tell your brain to move the finger. Then electrical communication within your body tells your nerves and muscles to move the finger. When there is disruption in the myelin sheath, those messages are weakened. Your brain is telling your finger to move but the nerves are damaged and the movement is weakened, delayed, or absent. When the myelin sheath is completely damaged, the message is blocked and this is called paralysis.
The disease can be present in a person for years prior to diagnosis. Because it is a gradually progressing disorder and its symptoms may, at early stages, wax and wane, a definitive diagnosis may require invasive tests. However, a neurologist that has experience in this type of disease should be able to identify the gradual symptoms and rule out any other cause. Typically, a diagnosis of CIDP is based on the person’s symptoms. Common symptoms in CIDP patients include:
In extremities:
- Pain
- Tingling
- Numbness
- Weakness
- Loss of deep tendon reflex
- Foot drop
- Difficulty walking (altered gait, stumbling)
- Fatigue
In addition to the aforementioned symptoms, tests such as a nerve conduction study (NCS) and electromyography (EMG) – a diagnostic procedure to assess the health of muscles and the nerve cells that control them – may be administered to determine the extent of demyelinating disease. In demyelinating disease, there is damage to the lining of the nerves that are critical for electrical nerve conduction. This can be confirmed by EMG studies or nerve biopsy. A nerve biopsy is used to confirm inflammatory process in the patient’s nerve.
A spinal fluid analysis is another diagnostic test that helps determine if a patient has elevated protein with normal cell count, an abnormality found in CIDP patients. Finally, your doctor may order blood and urine tests to rule out other disorders that may cause neuropathy, such as diabetes, which is the number cause of peripheral neuropathy.
The therapy for CIDP includes these three primary protocols:
- IVIG (intravenous immunoglobulin used to treat various autoimmune, infectious, and idiopathic diseases) – can aggravate kidney dysfunction, cardiovascular disease, cerebrovascular disease, and other.
- Corticosteroids (oral prednisone, pulse oral dexamethasone, IV methylprednisolone) – often improve strength, are conveniently taken by mouth, and are inexpensive. Side effects, however, can limit long-term use.
- Plasma exchange – a process by which some of the patient’s blood is removed and the blood cells returned without the liquid plasma portion of the patient’s blood. It may work by removing harmful antibodies contained in the plasma. Short-term relief.
If treated early, most CIDP people respond well to therapy that can reduce the damage to peripheral nerves and contribute to improved function and quality of life. If left untreated, 30% of CIDP patients will progress to wheelchair dependence.
In my next blog, I will discuss how CIDP can be service-connected, and how the VA evaluates CIDP for compensation.