Peripheral neuropathy is a common condition that can make daily tasks more challenging.
This condition often appears due to another condition, such as diabetes.
Former military service members who are living with peripheral neuropathy may be eligible for VA disability benefits.
In this post, we’re going over the VA rating for peripheral neuropathy.
What Is Peripheral Neuropathy?
According to the Merck Manual, peripheral neuropathy is “dysfunction of one or more peripheral nerves.”
In lay terms, neuropathy is commonly referred to as ‘nerve damage’ in the extremities.
Many veterans who are service connected for other disabilities also suffer from peripheral neuropathy; however, they have never been formally diagnosed with this condition.
Symptoms of Neuropathy
The Merck Manual lists the following symptoms of neuropathy:
- sensory disturbances
- pain
- muscle weakness and atrophy
- diminished deep tendon reflexes
- vasomotor symptoms.
Does VA consider peripheral neuropathy a disability?
While the VA does not have an exact diagnostic code for peripheral neuropathy, they do rate the condition based on the nerves affected by your specific neuropathy.
Below we will detail how the VA rates peripheral neuropathy and some common causes frequently seen from military service and veterans.
What is the VA Disability Rating for Peripheral Neuropathy?
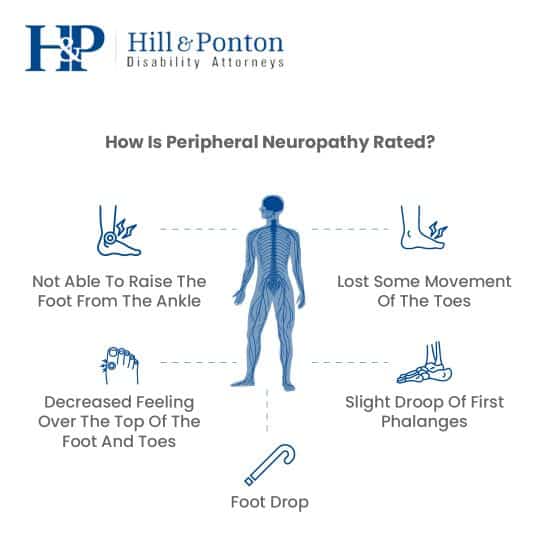
Peripheral neuropathy is rated by the VA based on the specific nerves affected since there’s no distinct diagnostic code for it.
The maximum standard rating is 40%, with the possibility of higher ratings for severe cases affecting multiple limbs.
To qualify for service-connected benefits, veterans must demonstrate their symptoms align with VA criteria for nerve damage, such as damage to the peroneal, sciatic, or femoral nerves.
Damage to these nerves might be rated under specific diagnostic codes, considering factors like foot drop, toe movement impairment, and sensory loss.
VA Ratings for Peripheral Neuropathy
- 10% – Minor sensory loss, slight movement impairment
- 20% – Noticeable movement and sensory impairment, limited foot/toe mobility
- 30% – Significant movement loss, severe sensory impairment
- 40% – Complete foot drop, inability to move foot at ankle, all toes drooping, significant loss of toe movement, substantial sensory loss over foot and toes
Veterans must communicate all symptoms to their physician for an accurate assessment.
Proper diagnosis, particularly for conditions like diabetes mellitus which may be related, is crucial for receiving deserved compensation.
Types of Neuropathy: Mononeuropathy and Polyneuropathy
Neuropathies are typically classified according to the problems caused or the root of the damage.
This is where we get the terms of mononeuropathy and polyneuropathy.
- Mononeuropathy is damage to a single peripheral nerve. Physical injury or trauma is the most common cause. Mononeuropathy can also be caused by prolonged pressure on the nerve, extended sedentary periods or continuous repetitive motions. Carpal tunnel is a common type of mononeuropathy caused by overuse strain on the nerve that passes through an individual’s wrist. The damage can cause numbness, tingling, pain, and unusual sensations in the first three fingers on the thumb side of a person’s hand.
- Polyneuropathy is damage to multiple peripheral nerves throughout the body. It makes up the greatest number of peripheral neuropathy cases. Polyneuropathy has a wide variety of causes which include:
- Exposure to toxins such as Agent Orange,
- Volatile organic compounds (such as those in the water at Camp Lejeune), and
- Alcohol abuse.
Common Causes of Peripheral Neuropathy in Veterans
The causes of peripheral neuropathy can be divided into three distinct categories: Acquired, hereditary, and Idiopathic neuropathies.
- Acquired neuropathies are caused by environmental factors (and are what a veteran would attempt to get service connected). Environmental factors which could cause neuropathy are toxins, trauma, illness, and infection. Know causes included:
- Diabetes
- Alcoholism
- Poor nutrition or vitamin deficiency
- Certain cancers (or their related chemotherapy treatment)
- Overly aggressive immune system damage
- Certain medications
- Kidney or thyroid disease
- Infections such as Lyme disease, shingles, or AIDS
- Hereditary neuropathies are less common. As the name indicates, these neuropathies are passed from parent to child. The most common is the Charcot-Marie-Tooth disease.
- Idiopathic neuropathies cause is unknown. Almost one-third of neuropathies are classified this way.
How do you prove peripheral neuropathy to VA?
Veterans should ensure thorough documentation of symptoms and pursue diagnostic tests like EMGs, NCVs, and biopsies for a solid claim foundation.
Challenges in diagnosing peripheral neuropathy often stem from underreported symptoms due to their intermittent nature, misconceptions about aging, or reluctance to seek medical help to avoid being labeled as complainers.
VA benefits for Delayed onset peripheral neuropathy
Misdiagnosis or undiagnosed peripheral neuropathy often stems from:
- Medical professionals not thoroughly listening to veterans’ nerve pain complaints.
- Failure to conduct essential diagnostic tests.
- Overlooking delayed-onset neuropathy that appears years post-service.
- Budget or time constraints affecting quality of care.
These issues can prevent veterans from accessing deserved benefits.
It’s vital for veterans to insist on comprehensive medical evaluations and the necessary tests for an accurate diagnosis and assessment of neuropathy’s severity.
How To Prove Peripheral Neuropathy Secondary to Diabetes
Peripheral neuropathy, particularly stemming from diabetes, is a significant concern for veterans.
As of 2021, 38.4 million Americans (roughly 11%) were diagnosed with diabetes, with an additional 86 million Americans aged 20 and older being pre-diabetic, numbers that have likely increased.
Veterans receiving compensation for diabetes mellitus from the VA may also qualify for disability compensation for conditions secondary to diabetes, divided into macrovascular (large blood vessels) and microvascular (small blood vessels) diseases.
Macrovascular diseases include conditions like coronary artery disease and stroke, affecting large vessels like the coronary arteries and aorta.
Microvascular diseases impact small vessels such as capillaries and include complications like retinopathy, nephropathy, and neuropathy.
Diabetic neuropathy, a common microvascular complication, manifests as nerve damage over time due to prolonged high glucose levels damaging the blood vessels that support nerves.
Diabetic neuropathy types include:
- Peripheral neuropathy (most common, affecting extremities)
- Autonomic neuropathy (affects the autonomic nervous system, impacting internal organs)
- Proximal neuropathy (impacts hips, buttocks, thighs)
- Focal neuropathy (targets specific nerves or nerve groups)
Veterans should seek a medical diagnosis and present records to the VA to potentially receive additional disability benefits for secondary conditions related to diabetes, including various types of neuropathy.
Peripheral Neuropathy Presumptive to Agent Orange Exposure
It’s important to note that peripheral neuropathy is one of the medical conditions that the VA has connected to Agent Orange exposure.
Medical evidence has shown that herbicides like Agent Orange can damage the nervous system.
If you are a Vietnam veteran, meet the criteria for Agent Orange presumption, and are living with peripheral neuropathy, you will automatically be eligible for VA disability compensation.