Along with PTSD, medical issues like Gulf War Syndrome and COPD are marching up the ranks in prevalence today. Gulf War Syndrome, a medically unexplained multi-symptom disease, deserves its own regulation really with how complex it can be. In this previous post, we gave a general overview of Gulf War Syndrome and how to obtain active duty service connection by presumption. Here we will discuss a specific ongoing issue: obtaining service connection from the Department of Veterans Affairs for Chronic Obstructive pulmonary disease or COPD as related to the inhaling of toxic fumes emitted from large fires.
The Gulf War Phases and Timeline
From a legal and medical standpoint, the 1991 Gulf War presented a unique set of challenges. Veterans who served in these eras have experienced health issues such as COPD, emphysema, fatigue, headaches, joint pain, chronic bronchitis, indigestion, insomnia, dizziness, respiratory disorders (COPD) from burn pits and environmental exposures, and memory problems. Sometimes they call it Gulf War Syndrome. Let’s get into it next down.
The first Gulf War, led by U.S. and coalition troops in January 1991, followed the August 1990 Iraqi invasion of Kuwait. The war was over on February 28, 1991, and an official cease-fire was signed in April 1991. Fourteen years later, Operation Iraqi Freedom (2003-2010) and Operation New Dawn (2010-2011) created a new group of persian Gulf War Veterans.
With President Obama’s announcement on August 31, 2010, the US combat mission in Iraq (Operation Iraqi Freedom) had officially ended, and with that, the second phase of the Gulf War.
How is Gulf War Syndrome different from COPD?
What makes Gulf War Syndrome unique is the inability of medical professionals to diagnose these symptoms. As a result, the VA and department of defense established 38 CFR §3.317, which more clearly defines the parameters of “undiagnosed illnesses” and the guidelines for receiving compensation for those illnesses.
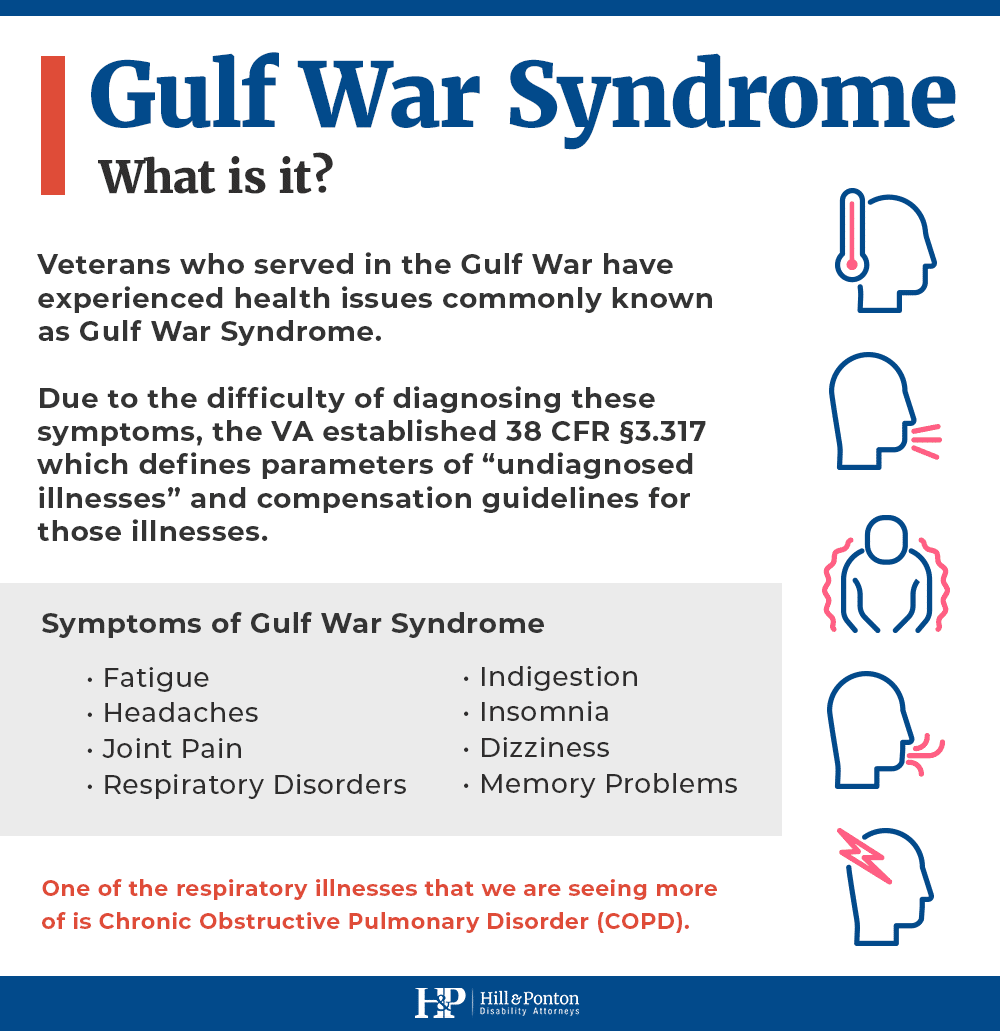
COPD, on the other hand, is one that can be diagnosed medically and we are are seeing more of Chronic Obstructive Pulmonary Disorder because of these burn pits and older oil fires.
COPD falls under respiratory conditions and is an obstructive lung disease characterized by chronically poor airflow. It typically worsens over time.
In contrast to asthma, medication does not significantly improve airflow or respiratory symptoms. While the primary cause of COPD is considered to be tobacco smoke, COPD can also be caused by occupational exposures and pollution from indoor fires (in some countries).
Common Symptoms of COPD
Some of the characteristics of COPD include:
- Shortness of breath, especially during physical activities
- Wheezing
- Chest tightness
- Sinusitis
- Rhinitis
- Having to clear your airway first thing in the morning, due to excess mucus in lungs
- A chronic cough that produces sputum that may be clear, white, yellow or greenish
- Blueness of the lips or fingernail beds (cyanosis)
- Frequent respiratory infections
- Lack of energy
- Unintended weight loss (in later stages)
- Exacerbations—severe episodes during which symptoms become worse and persist for days or longer
Service members who spent time in Kuwait or Saudi Arabia in 1991 will remember the huge billows of smoke and the smog that hung over the ground as over 600 oil wells burned for seven months.
Hundreds of US soldiers, national guard, and us army worked around those fires, breathing in particulate matter with little or no protection. Years later, the breathing problems they developed in Kuwait have only gotten worse.
While the Veterans Administration has declared that there is no evidence of long-term health problems from exposure to oil well fires at this time, the health problems of veterans who served in Kuwait tell another story.
Since COPD is not on the list of presumptive diseases associated with Gulf War Syndrome, it is more difficult of veterans to get service-connection for conditions outside this list.
COPD and Agent Orange Exposure
In addition to burn pits, Agent Orange could also contribute to a COPD diagnosis particularly with Vietnam-era Veterans. Agent Orange is a herbicide sprayed by the US military on foliage and US service members on the Vietnam landmass during the Vietnam War.
These “tactical herbicide” weapons cause severe chronic diseases including cardiovascular abnormalities , respiratory issues, skin conditions, diabetes, and much more.
How COPD is Rated
Under 38 USC §1117(g)(8) and 38 CFR §3.317 (b)(8), “signs or symptoms that may be a manifestation of an undiagnosed illness or a chronic multisymptom illness include: […] signs or symptoms involving the upper or lower respiratory system”.
COPD is common but it can be difficult to connect to service for your disability claim. In the news release dated September 28, 2010, the VA stated that, “for non-presumptive conditions, a Veteran is required to provide medical records to establish an actual connection between military service in Southwest Asia or Afghanistan and a specific disease”.
In order to be successful in establishing service-connection for conditions such as COPD, it is beneficial for vets to get an outside medical opinion on the matter such as a pulmonary function test. The VA is required to consider the evidence of medical opinions outside of the VA.
If the opinion of the independent medical practitioner is positive, the VA will be looking for the phrase “at least as likely as not”. If this phrase is not included in the report, or something to the equivalent, the VA will not make a favorable decision on the claim based upon that report.