If you’ve ever played a game of tug-of-war, you know how it feels to pull on a rope, your feet digging into the ground, the strain of your muscles as you try to move the other team.
Now imagine, you’re not tugging against another team, but against something invisible and heavy that sits inside of you.
This is often how it feels for many of our brave veterans when they grapple with mental health issues post-service.
Our veterans, those who served our country so selflessly, face a unique set of challenges when it comes to mental health.
The battlefield might be far away, but the mental scars and memories can remain, showing up in conditions like post-traumatic stress disorder (PTSD), depression, anxiety and other mental health issues.
In fact, all of the aforementioned disorders are pretty common among the community.
Did you know that nearly 1 in 4 veterans are diagnosed with at least one mental health disorder?
That’s like saying, in a class of 24 students, six are facing mental health challenges.
Yet, not all our veterans are getting the help they need to thrive–but, why?
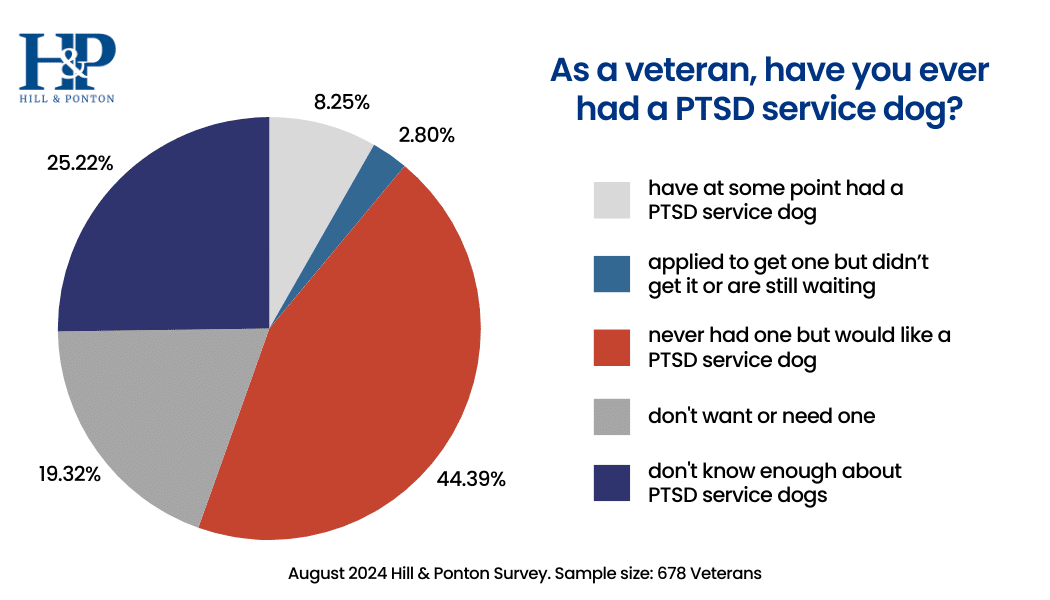
Through a mental health care survey conducted by disability law firm Hill & Ponton, which polled a community of over four hundred veterans, we discovered an overwhelmingly common answer to this question.
One of the biggest reasons our veterans aren’t seeking help for their mental health concerns?
The lack of accessibility of treatment.
Our survey, while highlighting a wide variety of considerations as to why veterans often didn’t pursue treatment, focused on these specific accessibility-related factors, most importantly:
- The veterans accessibility to a knowledgeable provider
- The availability and timeliness of care for the veteran
- The veterans knowledge of treatment options available
When we talk about the importance of mental health care for veterans, it’s vital to understand that simply having services available isn’t enough. To truly support our veterans, we need to consider whether these services are easily accessible to them.
There are a variety of factors that can make it hard for a veteran to get the mental health care they need. This part of our discussion focuses on these challenges, to better understand what might be standing in the way of a veteran and the care they deserve.
Finding a Provider with Knowledge of Military Culture
The understanding of military culture by mental health providers is a crucial aspect of ensuring effective and sensitive mental health care for veterans.
Our survey demonstrated that veterans place great importance on receiving mental health treatment from providers who have knowledge and background in military culture [1].
This understanding not only builds trust and rapport between veterans and their providers but also helps address the unique challenges and experiences that veterans may face.
Importance of Provider Understanding of Military Culture
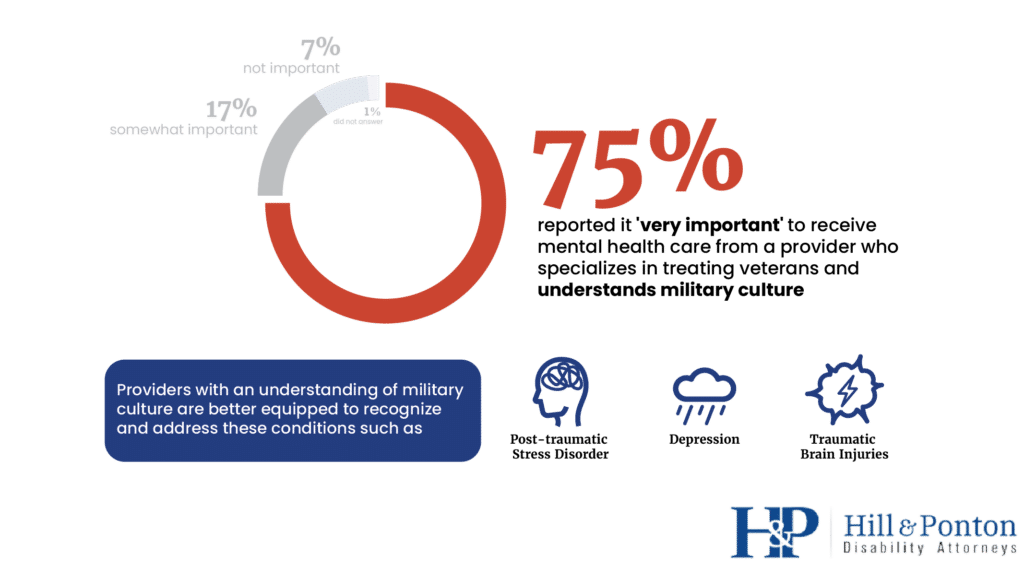
According to the survey, an overwhelming 75% of respondents reported it ‘very important’ to receive mental health care from a provider who specializes in treating veterans and understands military culture [1].
This highlights the significance of cultural competence among mental health professionals when working with veterans.
Veterans often encounter mental health issues specific to their military service, such as post-traumatic stress disorder (PTSD), depression, and traumatic brain injuries (TBI).
Providers with an understanding of military culture are better equipped to recognize and address these conditions effectively [2].
Challenges When Provider Lacks Military Cultural Competence
When mental health providers lack military cultural competence, veterans may face various challenges in their treatment journey.
Misunderstandings and misinterpretations of military experiences can lead to incorrect diagnoses and ineffective treatment approaches.
Veterans may also feel uncomfortable or hesitant to discuss sensitive military-related issues, affecting the therapeutic alliance and treatment outcomes [3].
Addressing Provider Understanding of Military Culture
Incorporating military cultural education and training in mental health provider curriculums can increase awareness and understanding of veterans’ unique experiences.
Training should cover the military’s structure, deployment experiences, common mental health challenges, and potential treatment approaches.
Establishing mentorship programs that pair experienced mental health providers with those who are new to working with veterans can be beneficial.
These programs can help share insights and knowledge about military culture and provide guidance on how to best approach veterans’ mental health care.
Encouraging veterans to provide feedback on their experiences with mental health providers can help identify areas for improvement.
Involving veterans in the selection process of mental health providers can also ensure that veterans have a say in receiving care from providers who are sensitive to military culture.
Adopting a veteran-centered care approach emphasizes the importance of cultural competence and tailoring treatment plans to address veterans’ unique needs.
This approach emphasizes collaboration and respect for veterans’ experiences and preferences in their mental health care journey.
Mental health providers should participate in ongoing professional development and continuing education to stay current with best practices in working with veteran populations.
This includes attending workshops, conferences, and webinars that focus on military cultural competence.
Ensuring Prompt Access to Mental Health Services for Veterans
Availability and timeliness of mental health care are vital factors that significantly impact veterans’ ability to receive timely and effective support for their mental health needs.
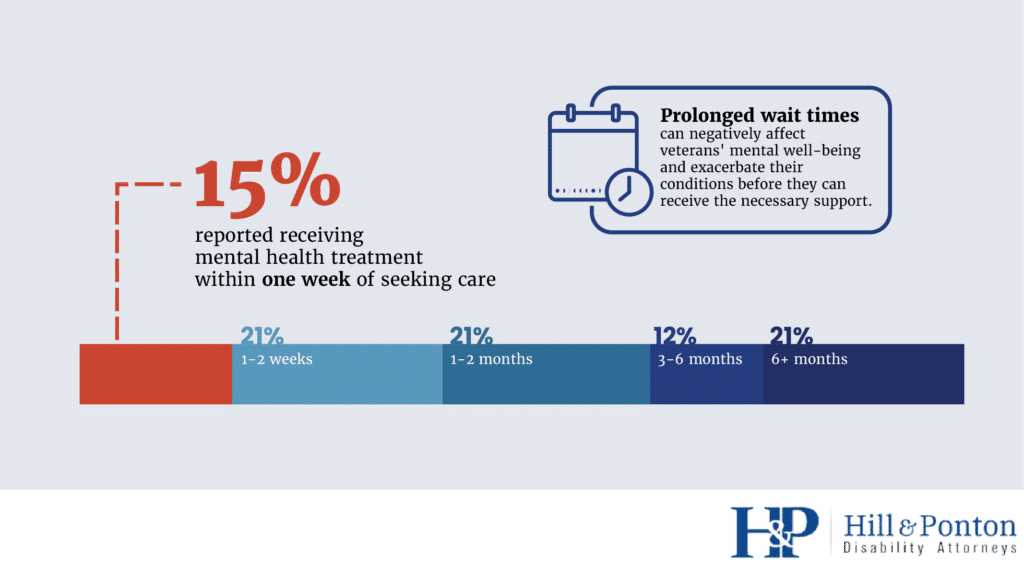
Our survey revealed key insights into the challenges veterans face in accessing mental health services promptly, emphasizing the need for improved availability and reduced wait times.
Challenges in Availability and Timeliness of Care
According to the survey, approximately 58% of veterans reported they were currently receiving mental health treatment for a service-connected disability [1].
While this indicates that a substantial number of veterans are accessing care, challenges persist in ensuring that mental health services are available to all veterans, especially those in underserved areas.
Limited Availability in Rural Areas
One of the primary barriers to timely mental health care for veterans is the limited availability of mental health providers in rural areas.
Veterans residing in remote regions often face difficulties in finding local mental health services.
The lack of nearby providers may necessitate long journeys or relocations to urban centers, further exacerbating the challenges veterans encounter in accessing care [2].
Long Wait Times for Appointments
Another significant issue is the extended wait times veterans experience when seeking mental health care.
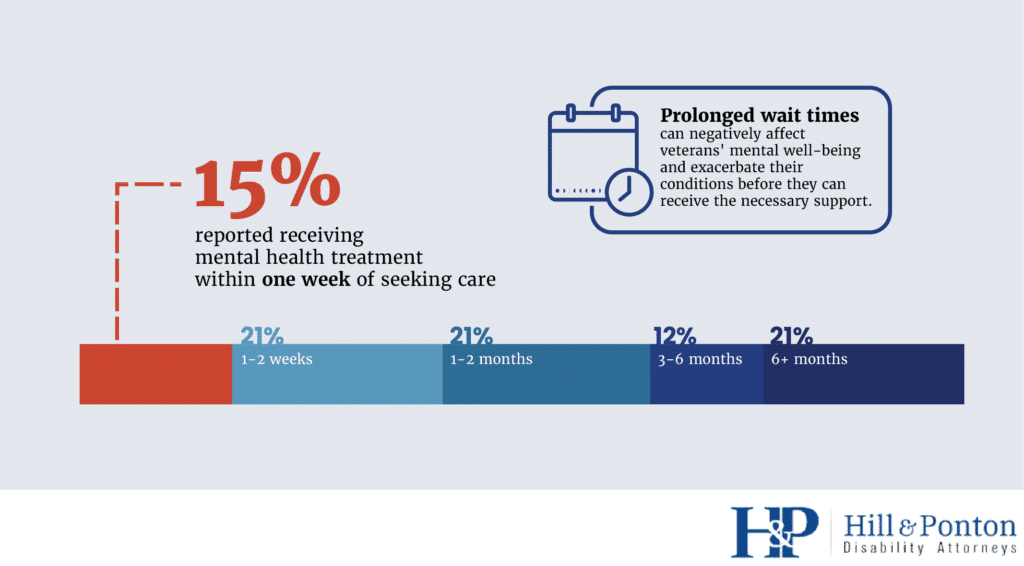
While 21% of respondents reported receiving treatment within one to two weeks of seeking it out, 20% had to wait more than six months [1].
Prolonged wait times can negatively affect veterans’ mental well-being and exacerbate their conditions before they can receive the necessary support.
Improving Availability and Timeliness of Care
Utilizing telehealth services can help overcome geographical barriers and increase mental health care accessibility for veterans in remote and rural areas.
Telehealth provides an avenue for veterans to connect with mental health providers remotely, reducing travel and wait times [3].
Efforts should be made to recruit and retain mental health providers who have expertise in working with veterans.
Incentives, such as loan repayment programs and competitive salaries, can attract providers to work in underserved areas and improve availability [4].
Establishing partnerships with community organizations and local healthcare providers can enhance mental health care access for veterans.
Community-based mental health initiatives can complement VA services, ensuring timely care for veterans in need [5].
Efficient coordination and communication among healthcare providers can reduce wait times for veterans seeking specialized mental health services.
Implementing streamlined referral processes can expedite access to necessary care [6].
Exploring innovative models of mental health service delivery, such as peer support programs and online counseling platforms, can increase the availability of mental health care options for veterans.
These alternative approaches can augment traditional face-to-face services [7].
Empowering Veterans with Informed Choices of their Treatment Options
Knowledge of available treatment options is a critical aspect of empowering veterans to make informed decisions about their mental health care.
In our survey, we found it was extremely important to provide veterans with comprehensive information about different treatment modalities and their potential benefits.
Awareness of Treatment Types
According to the survey, a substantial 42% of respondents reported not having tried any therapy types, suggesting that access to these therapies could be improved [1].
Cognitive Behavioral Therapy (CBT) emerged as the most common therapy type tried, but there remains a need to raise awareness about various other evidence-based therapies that can effectively address mental health conditions.
Value of Diverse Treatment Options
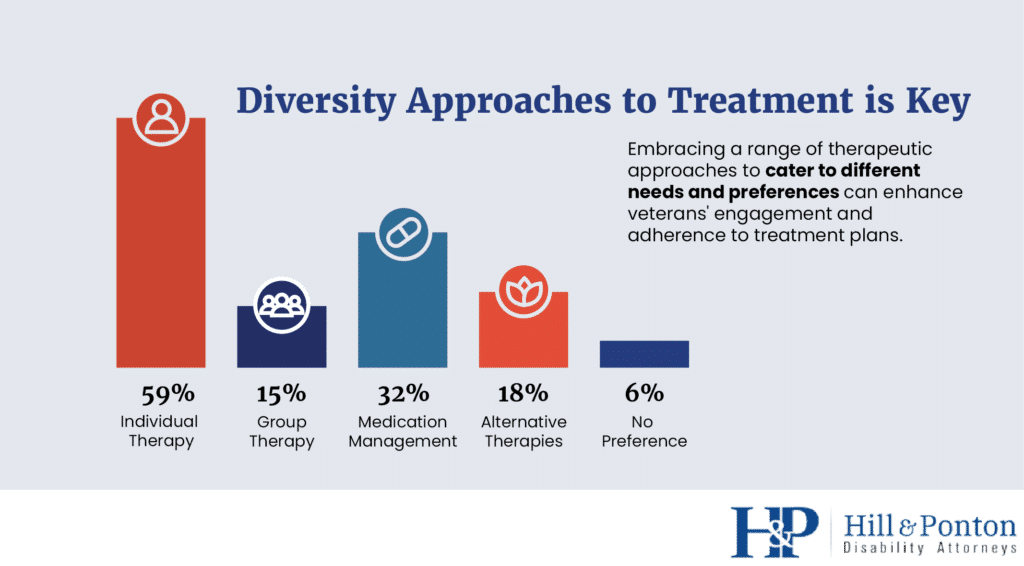
The survey also revealed that 18% of veterans expressed a preference for alternative therapies, such as yoga, meditation, or art therapy [1].
These findings underscore the significance of providing diverse treatment options to cater to different needs and preferences.
Embracing a range of therapeutic approaches can enhance veterans’ engagement and adherence to treatment plans.
Mixed Responses to Technology-Based Treatment
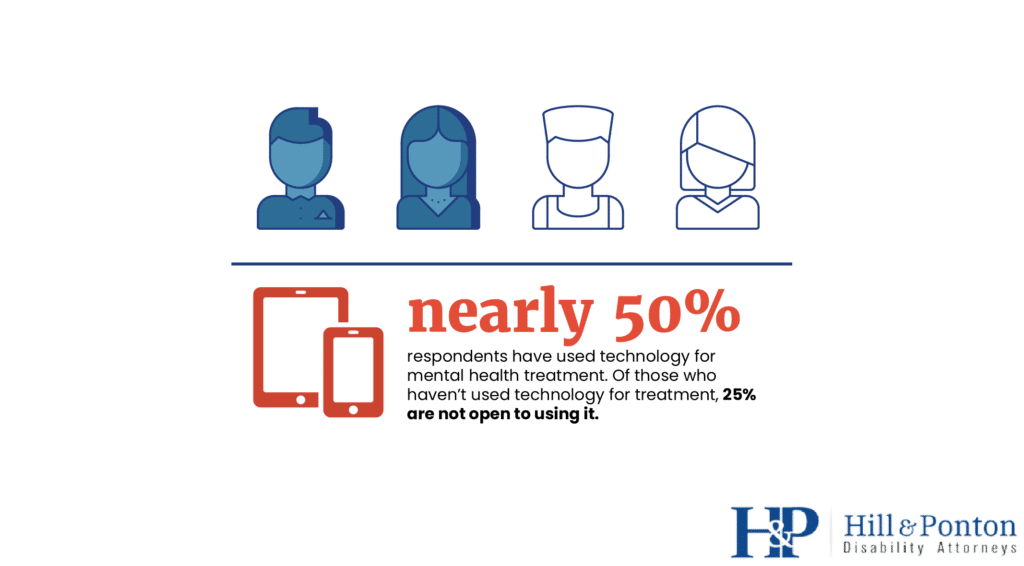
The use of technology for mental health treatment also had mixed responses in the survey.
While 32% of respondents expressed interest in trying technology-based mental health treatment but hadn’t tried it yet, only 9% found it more effective than traditional in-person treatment [1].
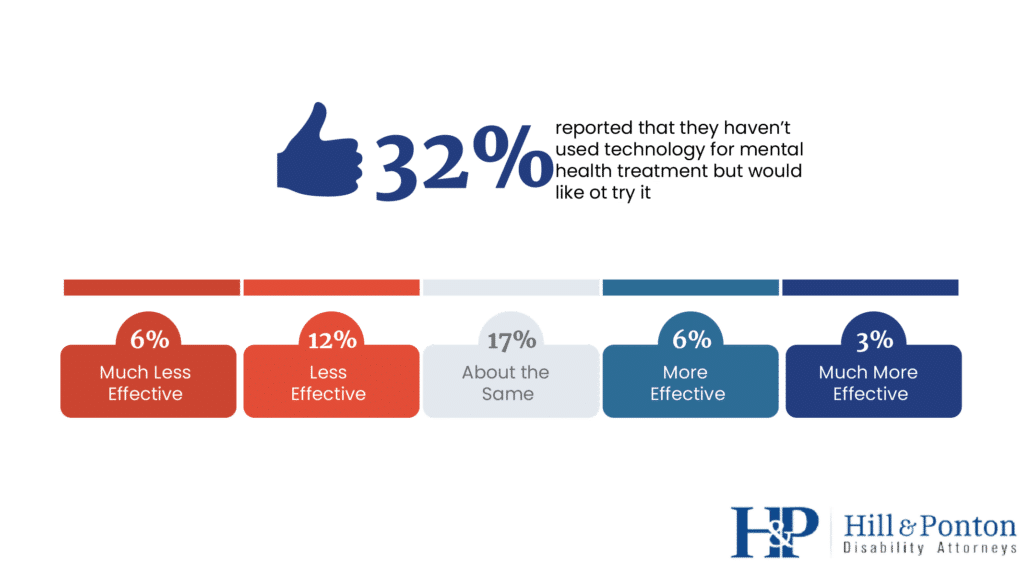
Understanding veterans’ views on technology-based interventions can inform the integration of digital mental health resources in their care.
Aiding in Veterans Knowledge of Treatment Options
Developing educational materials and resources that provide detailed information about various mental health treatment options can empower veterans to make well-informed choices.
These resources should be easily accessible and available in both digital and print formats.
Utilizing peer support programs and veteran mentoring can facilitate knowledge sharing among veterans.
Peers who have experienced various treatment approaches can provide valuable insights and support to those considering different therapies.
Promoting open and transparent communication between veterans and their mental health providers is essential.
Providers should take the time to discuss available treatment options, potential benefits, and any concerns veterans may have about specific modalities.
Integrating technology-based mental health resources into care can enhance veterans’ access to information and self-guided interventions.
Mobile apps, online portals, and virtual support groups can supplement traditional treatment approaches.
Methodology
To gain insights into veterans’ experiences with mental health treatment and identify factors influencing their access to care, we conducted a survey among a sample of 473 veterans.
The survey was designed and administered by Hill & Ponton, a VA disability law firm committed to understanding and advocating for the veteran community.
Survey Design
The survey was structured to collect comprehensive data on various aspects of mental health care access for veterans.
It consisted of approximately twenty main questions, covering topics such as current and past mental health treatment, preferred treatment methods, satisfaction with care, challenges in accessing care, and knowledge of treatment options.
Participant Recruitment
Participants for the survey were recruited from Hill & Ponton’s veteran audience mailing list.
The mailing list comprised veterans from diverse service backgrounds, representing a broad spectrum of experiences and needs.
The participants were invited to voluntarily participate in the survey to share their experiences and opinions related to mental health treatment.
Data Collection
Data collection for the survey was conducted through an online platform to ensure ease of access and participation for veterans.
Participants were provided with a unique link to access the survey, and responses were collected anonymously to maintain confidentiality and encourage candid feedback.
Data Analysis
Once the data collection period concluded, the responses were compiled and analyzed to extract valuable insights.
Quantitative data, such as percentages and frequencies, were calculated to summarize survey responses.
Additionally, qualitative responses were analyzed thematically to identify common patterns and sentiments expressed by veterans.
Survey Sample
The final sample size for the survey was 473 veterans.
This sample size was deemed sufficient to draw meaningful conclusions about the veteran community’s experiences with mental health care access and treatment preferences.
The participants represented a diverse range of service backgrounds, demographics, and geographic locations.
Limitations
While every effort was made to design a comprehensive and informative survey, certain limitations should be acknowledged.
Firstly, the survey relied on self-reported data from participants, which may be subject to recall bias or social desirability bias.
Secondly, as the survey was administered to a specific veteran audience mailing list, the findings may not be fully representative of the entire veteran population.
Lastly, while the survey provided valuable insights, it may not capture all potential factors influencing mental health care access for veterans.
Despite these limitations, the survey results offer valuable insights into veterans’ mental health care experiences and the factors that influence their access to treatment.
These findings provide a foundation for understanding the challenges veterans face and identifying potential avenues for improving mental health care accessibility and quality for those who have served our country.
Conclusion
In the journey toward better mental health for veterans, addressing accessibility factors is of paramount importance.
The understanding of military culture by mental health providers, the availability and timeliness of care, and knowledge of treatment options are critical pillars that shape veterans’ access to mental health services.
To ensure that every veteran has the support they need, we must prioritize providing mental health care from providers who are knowledgeable about military culture [2].
By expanding telehealth services and streamlining referral processes, we can overcome geographical barriers and reduce wait times for mental health care [3][6].
Empowering veterans with knowledge about various treatment options, including alternative therapies and technology-based interventions, allows them to actively participate in their mental health care journey [1].
As we continue to advocate for improved mental health services for veterans, let us strive for a future where every veteran has equitable access to the quality mental health care they need and deserve.
By embracing military cultural competence, enhancing availability and timeliness of care, and promoting knowledge of treatment options, we can create a mental health care system that truly supports our nation’s heroes.
References
- Data collected from the survey conducted by Hill & Ponton, a VA disability law firm.
- Blount, T. H., Sibold, J. S., Smith, W. L., & Bode, R. L. (2015). “Military Culture and Its Influence on Military Veterans’ Mental Health Care.” Professional Psychology: Research and Practice, 46(6), 424-432. https://psycnet.apa.org/doiLanding?doi=10.1037%2Fpro0000035
- U.S. Department of Veterans Affairs. (2023). “VA Video Connect: Connecting Veterans to Care.”
- VA Careers. (n.d.). “Loan Repayment.”
- Veterans Health Administration. (n.d.). “Community Care Overview.”
- Carretta, C. M., Wegener, S. T., & McDonell, M. B. (2013). “Wait Times for Veterans’ New Appointments as a Quality of Care Indicator.” Journal of Health Care Finance, 39(1), 39-50. https://pubmed.ncbi.nlm.nih.gov/24386517/
- Kuhn, E., Kanuri, N., Hoffman, J. E., Garvert, D. W., Ruzek, J. I., & Taylor, C. B. (2017). “A Randomized Controlled Trial of a Smartphone App for Posttraumatic Stress Disorder Symptoms.” JAMA Psychiatry, 74(5), 11-19.