For countless veterans, a restful night’s sleep remains elusive.
Sleep apnea, a common sleep disorder, affects a significant portion of our veteran community.
The National Veteran Sleep Disorder study reports that veterans are far more likely to experience obstructive sleep apnea compared to the general population.
This condition doesn’t merely disrupt sleep.
When left unchecked, it can have severe implications on one’s health, especially concerning heart disease.
For many, the connection between sleep apnea and heart disease might not be immediately apparent.
However, understanding this link is crucial, not just for overall health but also for maximizing VA disability benefits and ratings.
Sleep apnea manifests when breathing sporadically halts during sleep.
These pauses, which can range from a few seconds to minutes, often result in the person gasping for air, leading to disrupted sleep.
The impacts of sleep apnea aren’t confined to nighttime; they extend to daily activities, affecting mental health, energy levels, and attention spans.
Even more concerning is the potential of sleep apnea to elevate the risk of high blood pressure and, subsequently, heart disease.
Veterans, in their pursuit of rightful VA disability compensation, must be proactive about recognizing the signs of sleep disorders and their potential secondary conditions.
Such awareness can significantly impact their VA rating, benefits, and overall quality of life.
Understanding Sleep Apnea
Sleep apnea is characterized by repeated pauses in breathing during sleep.
It can occur hundreds of times a night, especially in severe cases, disrupting restful sleep.
Symptoms and Signs
- Loud snoring: A common symptom, particularly in cases of obstructive sleep apnea.
- Breathing cessation: Moments when one stops breathing during sleep, often noticed by a partner.
- Abrupt awakenings: Suddenly waking up gasping for air, typical of central sleep apnea.
- Morning discomfort: A dry mouth or sore throat upon waking.
- Sleep disturbances: Insomnia or frequent wakefulness.
- Daytime symptoms: Excessive fatigue, focus challenges, and mood changes.
Beyond Obesity
While obesity can increase the risk due to throat fat, anyone, regardless of weight, can develop sleep apnea.
Many medical conditions, from heart failure to PTSD (a condition many veterans face), can intensify its risk and symptoms.
Understanding sleep apnea’s prevalence among veterans and its links to other conditions is vital for both health and securing appropriate VA disability benefits.
To dive deeper into heart disease and how it pertains to VA ratings, check out our blog post on it below!
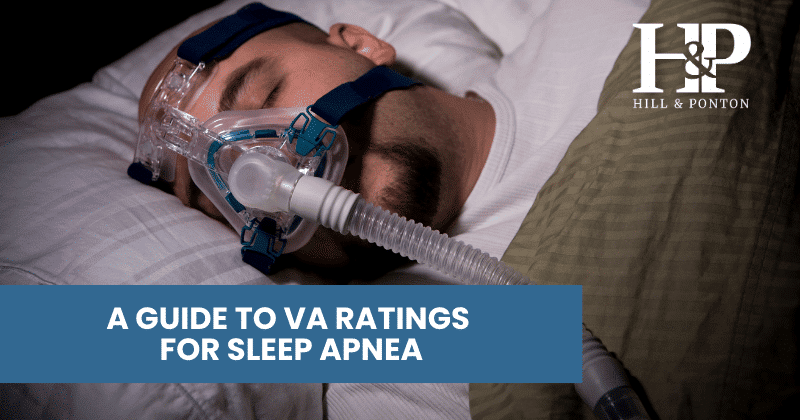
VA Disability Rating for Sleep Apnea
Heart Disease in Veterans
Heart disease is a significant concern for many, including veterans, particularly those with sleep disturbances like sleep apnea.
What is Heart Disease?
Heart disease encompasses a range of issues affecting the heart and its vessels.
It is responsible for numerous deaths in the U.S., covering conditions from coronary artery disease to arrhythmias and heart valve problems.
Symptoms and Common Indicators
- Chest discomfort: Often feels like pain, tightness, or pressure in the chest.
- Shortness of breath: Difficulty breathing during regular activities or while resting.
- Palpitations: Irregular heartbeats or a sensation of “fluttering”.
- Weakness or dizziness: Feeling light-headed or sudden dizziness can indicate heart issues.
- Pain in the arm: Particularly linked with conditions like angina.
- Swelling: Often observed in the legs, ankles, and feet, suggesting heart failure.
Risk Factors and The Sleep Apnea Connection
While factors like genetics and lifestyle choices play a role, the link between sleep apnea and heart disease is of particular relevance to veterans.
Obstructive sleep apnea causes breathing interruptions, leading to reduced oxygen in the blood and elevated blood pressure.
This consistent high blood pressure, or hypertension, increases risks like strokes and heart attacks.
A study even found individuals with severe obstructive sleep apnea had a 140% greater risk of heart failure, 60% risk for stroke, and 40% for coronary heart disease.
The relationship between sleep apnea and heart disease underscores the importance of timely diagnosis and treatment, not just for better sleep but also to safeguard heart health.
To learn more about heart disease and how it pertains to VA ratings, check out our blog post on it below!
VA Disability Rating for Heart Disease
The Relationship Between Sleep Apnea and Heart Disease
When diving deeper into the connection between sleep apnea and heart disease, it becomes apparent that the two conditions are closely intertwined.
Their relationship is one of cause and effect, where the complications of one exacerbate the risks of the other.
Medical Studies and Anecdotal Evidence
Numerous studies have underlined the alarming connection between sleep apnea and various heart conditions.
Research data indicates that veterans with severe obstructive sleep apnea are at a significantly increased risk of developing heart complications.
Beyond the realm of official research, there are countless anecdotes from veterans who’ve experienced both sleep disorders and subsequent heart problems.
Their experiences shed light on the often overlooked, yet deeply impactful relationship between breathing disturbances during sleep and cardiovascular complications.
Physiological Impacts
At the heart (pun intended) of this connection lies the body’s physiological response to disrupted breathing.
When a person with sleep apnea experiences an episode, their oxygen levels drop.
To counteract this, the body releases adrenaline and constricts blood vessels, pushing more oxygen to essential organs.
This, however, leads to an increase in blood pressure.
Continued episodes throughout the night mean the body is in a consistent state of heightened blood pressure, often spilling over into waking hours.
Over time, this becomes chronic hypertension, a leading factor behind various cardiovascular diseases.
The Danger of Night-time Blood Pressure
For most, blood pressure naturally drops by 10-20% during sleep.
However, sleep apnea sufferers undergo repeated spikes in blood pressure throughout the night due to their breathing interruptions.
The constant surges, much higher than normal, lead to systemic high blood pressure, even during the day.
Prolonged hypertension is a significant risk factor for many heart diseases, from stroke to heart attacks.
It’s clear that the relationship between sleep apnea and heart disease isn’t merely coincidental.
The physiological changes that occur during apnea episodes directly contribute to the onset of cardiovascular complications.
Recognizing this link is crucial, not just for veterans’ overall health, but also for securing the VA disability benefits that they rightfully deserve.
Interested in filing for heart disease secondary to sleep apnea but have been denied? Contact us today!

Why is Heart Disease Linked to Sleep Apnea?
While we’ve touched upon the immediate physiological responses that connect sleep apnea and heart disease, it’s crucial to delve deeper to truly grasp the profound interconnection.
Understanding these intricacies is not only vital for veterans’ health but also plays a pivotal role when addressing the scope of VA disability benefits.
Oxygen Deprivation and the Body’s Response
Central to the link between sleep apnea and heart disease is the body’s response to oxygen deprivation.
When breathing ceases during an apnea episode, oxygen levels in the bloodstream dip.
The brain, recognizing this threat, triggers a release of adrenaline—a hormone that prepares the body to respond to stress or danger.
Concurrently, blood vessels constrict to prioritize oxygen supply to vital organs.
Both these responses lead to a spike in blood pressure.
Inflammation and Endothelial Dysfunction
Sleep apnea can also contribute to systemic inflammation and endothelial dysfunction.
The endothelium is a thin layer of cells lining the inside of blood vessels.
Proper functioning is crucial for vascular health.
Disrupted sleep and intermittent oxygen shortage can cause this layer to function suboptimally, leading to cardiovascular problems.
Hormonal Imbalances
The constant waking during the night due to breathing interruptions and the subsequent lack of deep sleep can lead to hormonal imbalances.
Elevated cortisol levels, commonly referred to as the “stress hormone,” are often seen in sleep apnea patients.
Persistently high cortisol levels are associated with increased cardiovascular risks.
Stress on the Heart
Repeated episodes of low oxygen levels mean the heart must pump harder to circulate blood more effectively to compensate.
This added stress can exacerbate existing heart problems or pave the way for new ones.
Mental Health Implications
While not a direct physiological link, there’s an undeniable connection between sleep disorders and mental health.
Veterans with sleep apnea often experience anxiety, depression, or PTSD — conditions that can indirectly influence heart health.
The stress and mental strain contribute to hypertension and other cardiovascular risks.
Compounded Risks with Other Medical Conditions
Many veterans already grapple with other medical conditions that can either cause or be exacerbated by sleep apnea, such as traumatic brain injury, PTSD, and diabetes.
When combined with sleep apnea, the cumulative effect on heart health is substantial, creating a higher propensity for heart disease.
In summary, sleep apnea doesn’t merely pose risks as a standalone condition; it sets off a chain reaction of physiological events, hormonal changes, and mental health impacts.
These intertwined factors make the link between sleep apnea and heart disease in veterans a critical area of focus for personal health and the pursuit of adequate VA disability compensation.
Can Heart Disease Be Service Connected Secondary to Sleep Apnea?
Navigating the intricacies of VA disability benefits can often be a daunting task for our veterans.
However, it’s essential to understand the VA’s stance on service-connected conditions, especially when considering secondary conditions linked to primary diagnoses like sleep apnea.
The VA’s Perspective on Service-Connected Conditions
The Veterans Affairs recognizes the potential for primary service-connected conditions to lead to or aggravate secondary conditions.
A secondary condition is one that is directly caused or worsened by an already recognized service-connected condition.
Given the increasing evidence connecting sleep apnea and heart disease, the possibility of heart disease being acknowledged as a secondary condition to sleep apnea is gaining traction.
Proving Heart Disease Secondary to Sleep Apnea
Proving the connection between sleep apnea and subsequent heart disease is a pivotal step in achieving the rightful VA disability compensation for many veterans.
This journey may seem intricate, but with the right approach and understanding, it can be streamlined.
Gathering Robust Evidence
- Medical Records: Begin by collecting all pertinent medical records that indicate your sleep apnea diagnosis, its severity, and any heart-related complications or diagnoses.
- Sleep Study Results: Documented evidence from sleep studies can serve as definitive proof of sleep apnea severity, especially for obstructive sleep apnea cases.
- Treatment Histories: Document the treatments you’ve undertaken for both sleep apnea and heart disease. This can include CPAP or BiPAP machine usage records, medications, surgeries, or therapeutic interventions.
Want to know all the details about gathering evidence for claims? Read our blog post below.
The Key Types of Evidence in VA Disability Benefits Claims
Medical Documentation’s Role
A consistent medical documentation trail that traces the progression of your conditions over time is invaluable.
Records that show a worsening of heart condition in tandem with the presence or severity of sleep apnea can solidify your claim.
Seek Expert Opinions
Getting a professional opinion from specialists can dramatically boost your case.
Consider:
- Cardiologists: Their statements on how sleep apnea may have impacted your heart health.
- Sleep Specialists: They can provide insights into the severity of your sleep apnea and potential ramifications on overall health.
- Pulmonologists: Their expertise on respiratory issues and their implications on cardiovascular health can be instrumental.
Want to learn how to get the best nexus letter crafted for your claim? Read our guide below!
The Key to a Winning Nexus Letter
Monitoring and Consistency
Stay consistent in your medical monitoring.
Regular check-ups, consistent treatment, and diligent recording of symptoms and challenges can portray a clear picture of the connection between your sleep apnea and heart disease.
Personal Statements and Secondary Evaluations
While medical evidence is crucial, your personal narrative matters.
Detailed accounts of your daily struggles, the impact of both conditions on your life, and testimonies from loved ones can provide a comprehensive perspective.
Additionally, secondary evaluations from other medical practitioners or specialists can offer further insights into your condition and its implications.
The Role of Service Connection
Emphasize any potential incidents or exposures during your military service that could have contributed to or aggravated your sleep apnea.
This can further cement the service connection aspect of your claim, especially when paired with subsequent heart disease development.
In essence, proving heart disease as a secondary condition to sleep apnea in the realm of VA disability benefits boils down to a combination of solid medical evidence, expert opinions, personal narratives, and a clear portrayal of the service connection.
Armed with this holistic approach, veterans can better advocate for the compensation they rightfully deserve.
The journey for veterans to secure an appropriate VA disability rating that accurately represents their health challenges, especially when it comes to complex interconnected conditions like sleep apnea and heart disease, is crucial and deserving of attention.
Understanding the intrinsic link between sleep apnea and its potential to give rise to or exacerbate heart conditions can make a significant difference in the lives of many veterans.
The recognition of heart disease as a service-connected secondary condition to sleep apnea not only acknowledges the real health implications faced by veterans but also ensures they receive the rightful disability benefits.
Have Questions About Understanding How the Claims Process Works?
Hill & Ponton are here to support you with getting started with your claim.
If you are intending to appeal a denied claim, you can contact us for an evaluation and we can help you with this process.
However, if you are considering filing an initial claim, or even if you are interested in learning about the appeals process, we offer a free ebook to get you started on the right foot!
The Road to VA Compensation Benefits will help break down the claims process from start to finish. Click the link below to learn more.