Chronic obstructive pulmonary disease (COPD) is a lung disease that blocks the airways and makes it difficult to breathe. It causes the tubes and air sacs of the respiratory system to lose their elasticity, which causes them to expand and then traps some of the air in the lungs. The main cause of this respiratory failure is usually smoking, but diffusion capacity can also occur when people are exposed to harmful fumes in poorly ventilated areas or from bacterial infections.
How Does the VA Evaluate COPD?
The main symptoms for COPD include:
- Regular coughing
- Excessive phlegm
- Shortness of breath
- Wheezing
- Frequent and long-lasting colds
While it might be normal to be winded if you’re not used to physical exercise, someone with COPD will become short of breath even with simple chores. This condition is fairly common in terms of lung disorders, however it may be mistaken for chronic bronchitis, asthma, interstitial lung disease, or even lung cancer.
Chronic Obstructive Pulmonary Disease (COPD) is a general term used to describe a group of progressive lung conditions that cause airflow blockage and breathing-related problems. The VA recognizes and rates several distinct respiratory conditions that fall under the COPD umbrella:
- Chronic Bronchitis (Diagnostic Code 6600)
- Bronchiectasis (Diagnostic Code 6601)
- Asthma (Diagnostic Code 6602)
- Pulmonary Emphysema (Diagnostic Code 6603)
- Chronic Obstructive Pulmonary Disease (Diagnostic Code 6604)
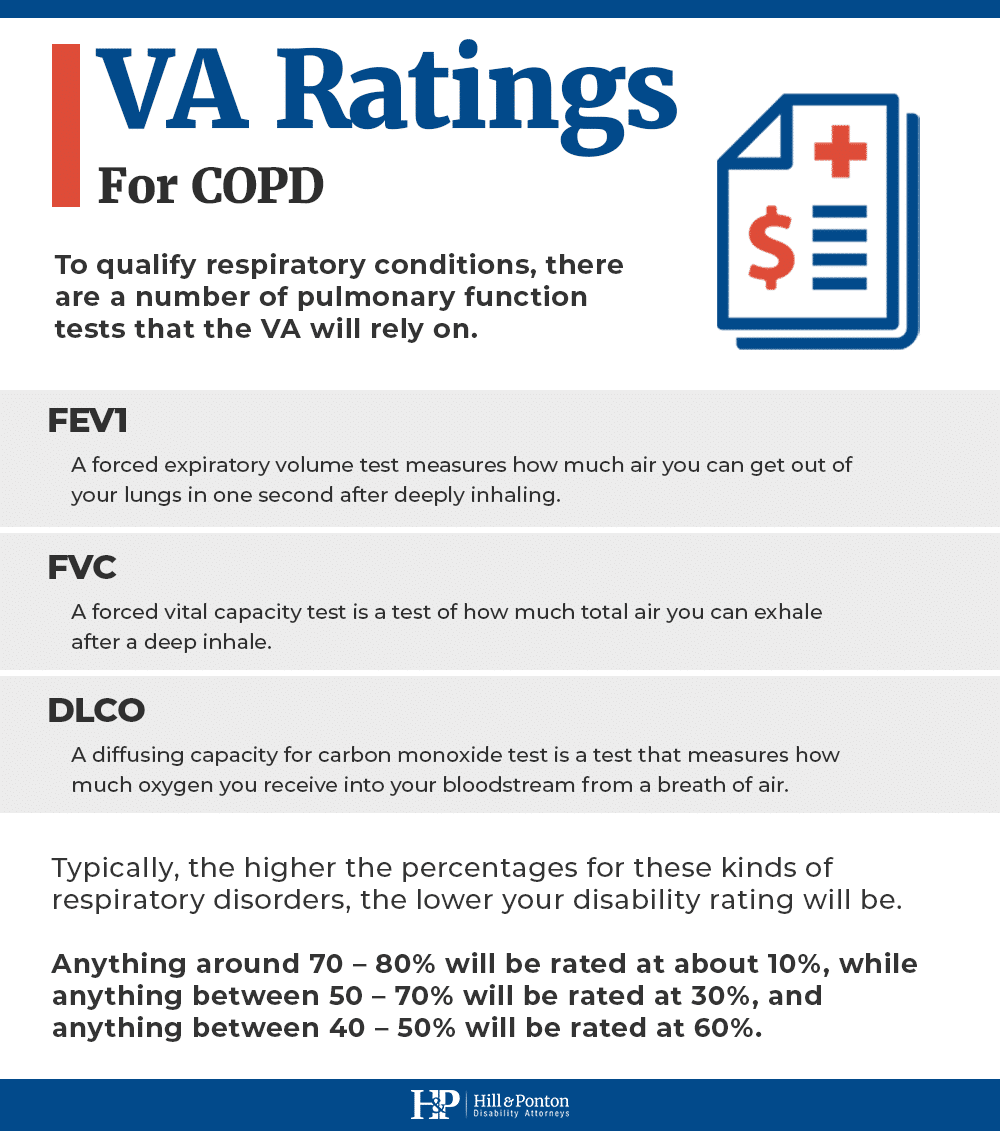
To qualify respiratory conditions, there are a number of pulmonary function tests that the VA will rely on. The FEV1 (forced expiratory volume) test measures how much air you can get out of your lungs in one second after deeply inhaling.
The FVC (forced vital capacity) is a test of how much total air you can exhale after a deep inhale (generally measured through spirometry). They may also consider your diffusing capacity for carbon monoxide (DLCO), a test that measures how much oxygen you receive into your bloodstream from a breath of air.
Typically, the higher the percentages for these kinds of respiratory disorders, the lower your disability rating will be. Anything around 70 – 80% will be rated at about 10%, while anything between 50 – 70% will be rated at 30%, and anything between 40 – 50% will be rated at 60%.
Keep in mind that the VA does not typically assign separate ratings for multiple respiratory conditions unless they affect different anatomical areas or result in distinct, non-overlapping symptoms. This is to comply with the anti-pyramiding rule.
What Is the VA Rating for COPD?
Under diagnostic code 6604, the VA disability rating for COPD is 10%, 30%, 60% or 100%, depending on the severity of the condition. The VA evaluates how long it takes the veteran with COPD to breathe, how much air they’re inhaling, how much air they’re exhaling, and the capacity to exercise.
- 100% rating: FEV-1 < 40%, or FEV-1/FVC < 40%, or DLCO < 40%, or maximum exercise capacity < 15 ml/kg/min with cardiorespiratory limitation, or cor pulmonale, or need for outpatient oxygen therapy
- 60% rating: FEV-1 40–55%, or FEV-1/FVC 40–55%, or DLCO 40–55%, or max exercise capacity 15–20 ml/kg/min
- 30% rating: FEV-1 56–70%, or FEV-1/FVC 56–70%, or DLCO 56–65%
- 10% rating: FEV-1 71–80%, or FEV-1/FVC 71–80%, or DLCO 66–80%
Pulmonary Emphysema Ratings
Emphysema (including panlobular, centrilobular and mixed) is a specific type of COPD where the air sacs in the lungs are damaged, reducing the lungs’ ability to transfer oxygen to the bloodstream.
Pulmonary emphysema is typically caused by long-term inhalation of toxins (e.g., smoking, chemical exposure) and is characterized by progressive shortness of breath and chronic fatigue due to reduced oxigenation.
The VA disability rating for pulmonary emphysema ranges from 10% to 30%, 60% and 100%, using the same rating criteria as COPD under a different diagnostic code (DC 6603):
- 100% rating: FEV-1 less than 40 percent of predicted value, or; the ratio of Forced Expiratory Volume in one second to Forced Vital Capacity (FEV-1/FVC) less than 40 percent, or; Diffusion Capacity of the Lung for Carbon Monoxide by the Single Breath Method (DLCO (SB)) less than 40-percent predicted, or; maximum exercise capacity less than 15 ml/kg/min oxygen consumption (with cardiac or respiratory limitation), or; cor pulmonale (right heart failure), or; right ventricular hypertrophy, or; pulmonary hypertension (shown by Echo or cardiac catheterization), or; episode(s) of acute respiratory failure, or; requires outpatient oxygen therapy.
- 60% rating: FEV-1 of 40- to 55-percent predicted, or; FEV-1/FVC of 40 to 55 percent, or; DLCO (SB) of 40- to 55-percent predicted, or; maximum oxygen consumption of 15 to 20 ml/kg/min (with cardiorespiratory limit)
- 30% rating: FEV-1 of 56- to 70-percent predicted, or; FEV-1/FVC of 56 to 70 percent, or; DLCO (SB) 56- to 65-percent predicted
- 10% rating: FEV-1 of 71- to 80-percent predicted, or; FEV-1/FVC of 71 to 80 percent, or; DLCO (SB) 66- to 80-percent predicted
Veterans may develop pulmonary emphysema from military occupational exposure to dust, smoke, or fumes. If your medical records say “emphysema” rather than just “COPD,” it may be better to file under DC 6603 (pulmonary emphysema) because it is more specific. If the diagnosis is broad (“COPD”), the VA will usually rate it under DC 6604. Both use the same rating schedule, but specificity may help in appeals and medical opinions.
Can You Get TDIU for COPD?
If your COPD (including pulmonary emphysema) significantly impairs your ability to work, you may qualify for a Total Disability Rating Based on Individual Unemployability, which pays at a 100% level, even if your schedular rating is less than 100%.
COPD’s progressive nature and limitation on physical activity (due to shortness of breath and fatigue) often make it a strong basis for TDIU claims. Learn more about VA unemployability.
Service Connecting COPD
Any kind of exposure to toxic air can cause COPD, so if you were exposed to gas, particulate matter, or Agent Orange during the service, you may be able to file for disability. Those who served in Afghanistan or Iraq may have been especially likely to file for VA disability benefits as they may have been asked to work near burn pits.
COPD is also a potential complication of adenovirus vaccines provided to military members from the 1960s until the 1990s. These vaccines were used to prevent acute respiratory disease (ARD), pharyngitis, conjunctivitis, and pneumonitis.
Service Connection Requirements
If you are filing for disability for COPD, you’ll need the following documents:
- A recent diagnosis of COPD from a qualified medical professional
- A description of how you came to be exposed to the chemicals that caused or aggravated your condition
- A letter (medical nexus) from your doctor that confirms your COPD was directly related to being in the military
Your COPD does not need to be caused by direct orders in the military. For example, even if you weren’t asked to work at the burn pits but did sleep nearby, you would still have the right to file for disability. There are several ways to establish that COPD is connected to military service:
Direct Service Connection
You must prove that an in-service event or exposure caused your COPD. For example, if you served in a role with frequent exposure to dust, chemicals, or burn pits, and later developed COPD, a strong nexus letter from a pulmonologist can significantly improve your disability claim’s success rate.
Secondary Service Connection
COPD may also develop as a result of another service-connected condition. For COPD, it could be asthma, bronchitis, an infection or anything else that would cause or worsen the condition. You will have to get an opinion from your doctor or medical professional to show that they agree with your chain of logic.
For example, if you developed PTSD directly because of your time in the military, the stress might have led you to take up smoking to calm your nerves. The military does allow you to make the connection if your smoking led to COPD, although this remains difficult to prove. You will need:
- A diagnosis of nicotine dependence resulting from a service-connected mental health condition
- Medical evidence linking COPD to that dependence
- An expert medical opinion supporting both elements
Due to the VA’s strict scrutiny in such cases, hiring a lawyer is highly recommended. If you were denied a VA disability rating for COPD caused by nicotine addiction, we may be able to help you – get a free case evaluation here.
Service Connection by Aggravation
This applies when COPD existed prior to being enlisted but was permanently worsened by military service. To get VA disability you will need:
- Clear evidence that COPD preexisted enlistment (e.g., medical records or entrance exam)
- Worsening of COPD beyond natural progression during service
- A medical opinion confirming the worsening and ruling out natural disease progression
Service Connection Based on VA Medical Malpractice
You may qualify for VA disability if the COPD or its worsening resulted from VA hospital care, surgery, or failure to diagnose or treat. The claim would have to be filed under 38 U.S.C. § 1151. Note that this type of claim can very difficult to win and typically requires legal representation.
Making a Successful Claim for COPD
To prepare your VA disability claim, gather the following:
- Results of your Pulmonary Function Tests (PFTs)
- Medical records diagnosing and treating COPD
- Nexus letter from your physician explaining the link between service and your condition
- Service records showing exposure to harmful substances
- Buddy statements, if applicable, verifying exposure
After you hand over all of your paperwork to the VA Regional Office, the committee will review it and most likely order a Compensation & Pension exam.
The C&P Exam for COPD
This exam is not meant to cure your COPD or even treat it. It’s performed by a VA doctor who will evaluate and verify your test results, symptoms, and the most likely cause of your condition.
The VA doctor will likely perform many of the same procedures as your primary physician. They might also make recommendations, such as using a bronchodilator to increase the capacity of the lung, oxygen therapy, or cardiac catheterization.
In some cases, the VA doctor will not agree with your primary or diagnosing physician. They may believe that you either have a different condition, such as pulmonary hypertension, bronchiectasis, or heart failure. Or they might decide that your COPD was not caused by your time in the military.
Should you want to contest the VA doctor’s conclusions, you can file an appeal, request that a higher authority look at the evidence or collect new evidence and submit it to the VA (e.g., a new X-ray, carbon dioxide labs, etc.).
If you’re asking for someone else to review the case, the idea is that it will be handed off to a different person, one with more experience in lung disorders. If you’re gathering new evidence, you’ll need to ensure that it’s supporting your COPD disability claim. Talking to your primary physician or a disability lawyer can make it easier to decide which evidence will help your case.
If you were denied VA disability benefits for COPD, consider getting assistance from our experienced attorneys. We’d be honored to help you obtain the benefits you’re entitled to.