Chronic insomnia, characterized by difficulty falling or staying asleep, or waking too early, is often triggered or worsened by the demands and aftereffects of military life. The VA recognizes the serious impact of sleep impairment and assigns disability ratings from 0% to 100% for insomnia shown to be connected to a veteran’s service. Hill & Ponton helps veterans establish service connection, meet VA rating criteria, and win the highest possible disability compensation for insomnia and related conditions.
How the VA Rates Insomnia
The Department of Veterans Affairs (VA) rates insomnia under the General Rating Formula for Mental Disorders in 38 CFR § 4.130, with ratings from 10% to 100%. A diagnosis of insomnia, without other concomitant mental disorders, typically receives, at least initially, a 30% rating for chronic sleep impairment. But insomnia is usually rated as a symptom of a service-connected mental disorder (e.g., PTSD, generalized anxiety disorder, depression, adjustment disorder), or under a secondary service connection theory when linked to a rated mental or physical condition. The rating percentages assigned to mental health disorders are:
- 0%: A mental condition has been formally diagnosed, but symptoms are not severe enough either to interfere with occupational and social functioning or to require continuous medication.
- 10%: Occupational and social impairment due to mild or transient symptoms which decrease work efficiency and ability to perform occupational tasks only during periods of significant stress, or symptoms controlled by continuous medication.
- 30%: Occupational and social impairment with occasional decrease in work efficiency and intermittent periods of inability to perform occupational tasks (although generally functioning satisfactorily, with routine behavior, self-care, and conversation normal), due to such symptoms as: depressed mood, anxiety, suspiciousness, panic attacks (weekly or less often), chronic sleep impairment, mild memory loss.
- 50%: Occupational and social impairment with reduced reliability and productivity due to such symptoms as: flattened affect; circumstantial, circumlocutory, or stereotyped speech; panic attacks more than once a week; difficulty in understanding complex commands; impairment of short- and long-term memory; impaired judgment; impaired abstract thinking; disturbances of motivation and mood; difficulty in establishing and maintaining effective work and social relationships.
- 70%: Occupational and social impairment, with deficiencies in most areas, such as work, school, family relations, judgment, thinking, or mood, due to such symptoms as: suicidal ideation; obsessional rituals which interfere with routine activities; speech intermittently illogical, obscure, or irrelevant; near-continuous panic or depression affecting the ability to function independently, appropriately and effectively; impaired impulse control; spatial disorientation; neglect of personal appearance and hygiene; difficulty in adapting to stressful circumstances; inability to establish and maintain effective relationships.
- 100%: Total occupational and social impairment, due to such symptoms as: gross impairment in thought processes or communication; persistent delusions or hallucinations; grossly inappropriate behavior; persistent danger of hurting self or others; intermittent inability to perform activities of daily living (including maintenance of minimal personal hygiene); disorientation to time or place; memory loss for names of close relatives, own occupation, or own name.
When Is Insomnia Rated Separately?
If insomnia exists only as a symptom of another service‑connected mental health condition (such as PTSD, anxiety, or depression), it is usually rated together with that condition under the General Rating Formula for Mental Disorders. However, if a clinician diagnoses chronic insomnia disorder or another distinct mental health condition and documents that it causes independent occupational or social impairment, it may be rated separately as a secondary condition if the Veteran is not service-connected for any other disability rated under the general rating formula for mental health disordersa.
This separation of ratings must comply with the anti‑pyramiding rule in 38 C.F.R. § 4.14, which prevents the VA from compensating the same symptom under multiple diagnoses. To justify a distinct rating, the evidence must show that insomnia produces unique, non‑overlapping functional limitations apart from the primary disability.
Service Connecting Insomnia
To receive VA compensation, veterans must prove that their insomnia is service-connected: that it either began during military service or was caused or aggravated by a service-connected condition. The VA calls this process establishing service connection, and it requires three things:
- A current diagnosis of insomnia by a qualified medical provider.
- Evidence of an in-service event or exposure (or, for secondary service connection, a separate service-connected condition) that caused or aggravated it.
- A medical nexus, or link, connecting your current insomnia to that in-service event or to another service-connected condition
A 2020 study published in Sleep found that 57.2% of post-9/11 veterans newly enrolling in VA health care met diagnostic criteria for insomnia disorder. In comparison, only about 30% of adults in the general population experience insomnia symptoms, with 6%–10% meeting the threshold for chronic insomnia disorder. This is because veterans face unique risk factors such as combat stress, deployment schedules, environmental exposures, and long-term pain. These factors make them twice as likely to experience chronic insomnia compared to civilians.
Is Insomnia a Presumptive Condition?
Insomnia is not classified as a presumptive condition under VA law. That means the VA does not automatically assume service connection and veterans must prove their insomnia began in service or was caused by another service-connected condition. However, some Gulf War veterans can still qualify for presumptive service connection when insomnia is part of a broader “medically unexplained chronic multisymptom illness” (MUCMI) under 38 CFR § 3.317.
Veterans who served in certain locations during the Persian Gulf War era and now experience chronic insomnia may be eligible for presumptive benefits. Under VA regulations, sleep disturbances are recognized as one of the key symptoms of MUCMIs (conditions with no clear medical cause but significant physical and psychological effects). You may qualify if you meet all of the following criteria:
- Service location in Southwest Asia or nearby operational theaters, such as Iraq, Kuwait, Saudi Arabia, Bahrain, Qatar, Oman, the UAE, or the neutral zone between Iraq and Saudi Arabia
- Time period from August 2, 1990, through the present, as VA still recognizes ongoing Gulf War-era service
- Chronicity – Sleep disturbance symptoms have lasted six months or longer
- Diagnosis exclusion – No identifiable medical cause explaining the insomnia (such as PTSD, sleep apnea, or depression)
If these criteria apply, VA can award benefits on a presumptive basis, meaning you don’t need to prove the exact cause of your insomnia. The presumption acknowledges that environmental exposures such as burn pits, oil fires, and desert dust are known to produce unexplained long-term symptoms, including insomnia. Keep in mind that even under the Gulf War presumption, documentation still matters. To build a strong claim, include:
- Deployment verification from your DD 214 or service personnel file.
- Medical evidence showing sleep problems that began after Gulf War service.
- Statements from family or peers confirming chronic fatigue, irritability, or restlessness since deployment.
- A medical nexus clarifying that your insomnia is part of a chronic, unexplained symptom cluster rather than another diagnosable disorder.
If VA denies your claim because they argue another diagnosis explains your symptoms, your representative can appeal by showing that the other condition (for example, chronic fatigue syndrome) does not fully account for the insomnia’s persistence or severity.
Other VA Presumptions That Can Help Service Connect Insomnia
- Toxic exposure presumptions under the PACT Act (2022) allow veterans exposed to burn pits, oil fires, or particulate matter to receive presumptive service connection for certain respiratory and systemic illnesses that can contribute to sleep disorders. If your insomnia stems from or is aggravated by one of those presumptive respiratory or neurological conditions, you may indirectly qualify through secondary service connection.
- POW presumption: Although rare, veterans held as prisoners of war may develop long-term anxiety and sleep disturbance symptoms that qualify as part of their presumptive psychiatric conditions under 38 CFR § 3.309(c).
VA will not presume insomnia by name, but it does recognize sleep disturbance as a chronic residual of deployment-related exposures and stress. Gulf War veterans and those covered by the PACT Act have the strongest presumptive pathway, while others must establish service connection directly or secondarily through another rated condition.
Direct Service Connection
A direct service connection means the VA recognizes that your insomnia began during, or directly because of, your active-duty service. Unlike presumptive or secondary service connections, this route requires specific proof linking your current insomnia diagnosis to an event, injury, or condition documented while serving. To establish a direct link, veterans need the three key elements forming the Caluza triangle:
- A current medical diagnosis of insomnia or “chronic insomnia disorder”
- An in-service event, injury, or stressor that likely caused or triggered the sleep disorder
- A nexus (medical opinion) connecting your current condition to that in-service event
Example of direct service connection: A veteran served two tours in Afghanistan as a vehicle mechanic exposed to constant noise and diesel fumes. STRs note frequent complaints of sleeplessness and anxiety. After discharge, VA medical records show a chronic insomnia diagnosis, with a psychologist’s nexus letter linking the disorder to “persistent hyperarousal related to deployment stress and environmental exposure.” Because every element of the diagnosis, in-service occurrence, and nexus was present, the veteran received a 30% rating for chronic sleep impairment under Diagnostic Code 9413.
Tips to Prove Direct Connection
- Document continuity. Show that sleep problems began in service and never fully resolved. Gaps in records weaken credibility. Statements from partners, roommates, or other people who have witnessed your insomnia firsthand can help fill in gaps when medical records are scarce.
- Use consistent terminology. Providers should label your condition “insomnia disorder” or “chronic insomnia,” not vague terms like “tiredness.”
- Emphasize functional effects. Explain how poor sleep causes errors, absenteeism, or family strain; functional loss drives the percentage awarded.
- Request your C-File (claims file). Reviewing your own service records helps ensure relevant notes aren’t overlooked during adjudication.
Establishing a direct connection is important because it provides the strongest legal foundation for your claim. Once the VA concedes direct service connection, you remain eligible for increased ratings and secondary conditions linked to insomnia (such as depression, hypertension, or chronic fatigue) without having to re-prove the original cause.
Secondary Service Connection for Insomnia
When the VA denies direct service connection because insomnia didn’t begin during active duty, you may still qualify under secondary service connection. Veterans often experience insomnia as part of a larger constellation of secondary mental health or physical issues. Conditions like chronic pain can severely impact a veteran’s ability to sleep, which in turn can worsen their overall health.
Secondary service connection is one of the most common paths for veterans seeking benefits for sleep disorders. The VA recognizes that chronic sleep loss often develops as a symptom of another physical or mental health condition. When your medical records show that insomnia worsened because of your already service-connected disability, you can receive compensation for both (keeping in mind that if the primary disability is rated under mental health criteria, insomnia can only contribute to a higher mental health rating instead of being rated separately). To win a secondary service connection, you must show:
- You have a current diagnosis of insomnia disorder
- You already have a primary service-connected condition (for example, lumbar spine degenerative joint disease)
- There is a medical nexus showing that your insomnia was either caused by or aggravated by that primary condition
This third step of the nexus is essential. A qualified clinician must provide a written opinion explaining how the primary condition directly contributes to your insomnia or worsens it beyond its normal progression.
Insomnia Secondary to Chronic Pain
Chronic pain is one of the leading causes of sleep deprivation among veterans. Chronic pain from service-connected injuries frequently disrupts sleep, creating a cycle where poor sleep worsens pain and leads to depression and anxiety. Pain medications, like morphine or codeine, can further disturb sleep patterns. Veterans with service-connected physical pain that causes insomnia may be eligible for a secondary VA disability rating, especially if a medical professional confirms the link between their pain and insomnia.
If you already have service-connected back or neck pain, a joint disease or any other condition that causes chronic pain, and your medical provider confirms that pain prevents restful sleep, you can pursue secondary service connection for insomnia. Evidence to include:
- Treatment records showing reports of difficulty sleeping due to pain
- Nexus letter linking chronic pain and sleep impairment
- Medication history, especially if painkillers or muscle relaxers interfere with normal sleep architecture
- Statements from family or roommates confirming visible fatigue or irritability
Insomnia and PTSD
PTSD and insomnia are deeply interconnected. Veterans with PTSD often experience nightmares, flashbacks, and anxiety that disrupt sleep, leading to avoidance of rest and heightened nighttime anxiety. This can worsen insomnia, making them more sensitive to noise and silence. Some may resort to alcohol or drugs to sleep, further harming their health. Since insomnia can be an extension of PTSD symptoms, veterans may qualify for a higher VA mental health rating, as sleep disturbances like insomnia can limit social and occupational functioning.
Can you get a rating for insomnia secondary to PTSD? Because insomnia is often a core symptom of PTSD, it’s usually considered part of the PTSD rating under Diagnostic Code 9411. However, if a veteran’s sleep disturbance causes separate, measurable impairment such as severe fatigue or cognitive decline, they may qualify for a higher combined mental health rating.
Insomnia Secondary to Tinnitus
For veterans with tinnitus, the constant ringing or buzzing in the ears, insomnia is a frequent secondary issue. The persistent noise often prevents sleep onset and causes stress-related hyperarousal. Evidence that supports a tinnitus-related claim:
- Audiology reports confirming tinnitus diagnosis
- Sleep logs or treatment notes linking difficulty sleeping to ringing intensity
- A nexus statement from an audiologist or ENT specialist explaining that tinnitus aggravates or causes insomnia
- Documentation that lack of sleep further worsens tinnitus perception, creating a self-reinforcing cycle
Example: A veteran rated 10% for tinnitus submits a nexus letter from an ENT specialist stating, “The veteran’s tinnitus significantly disrupts sleep, producing persistent insomnia characterized by difficulty falling and staying asleep.” The VA approves service connection for insomnia secondary to tinnitus, resulting in a combined rating increase. Find out more about insomnia secondary to tinnitus.
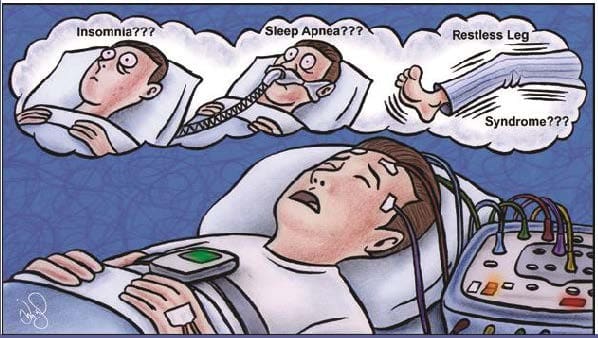
Sleep Apnea and Insomnia VA Ratings
Although both conditions interfere with sleep, insomnia and sleep apnea are distinct medical disorders, and the VA rates them differently. However, many veterans suffer from both, which can make claims more complicated. Understanding how the VA views their overlap is crucial to ensuring you receive full compensation.
Insomnia is a mental health–related sleep disorder characterized by difficulty falling asleep, staying asleep, or achieving restorative rest. It’s rated under the General Rating Formula for Mental Disorders in 38 CFR § 4.130. Sleep apnea, on the other hand, is a respiratory condition that causes repeated pauses in breathing during sleep. It’s rated under Diagnostic Code 6847 in 38 CFR § 4.97, with percentages ranging from 0% to 100% depending on the severity and treatment requirements. The VA rates sleep apnea based on severity and the medical interventions required:
- 0% – Diagnosis confirmed, but symptoms do not cause measurable functional limitation
- 30% – Evidence of persistent daytime hypersomnolence (excessive tiredness)
- 50% – Condition requires use of a CPAP machine or another breathing-assistance device during sleep
- 100% – Presence of chronic respiratory failure, cor pulmonale (right-sided heart strain), or the need for a tracheostomy
These ratings are objective and equipment-based, unlike insomnia ratings, which depend on how symptoms affect occupational and social functioning. You can be rated for both only when medical evidence shows each condition independently contributes to functional impairment. The VA will not award two separate ratings if one condition’s symptoms overlap with or duplicate the other’s “pyramiding” under 38 CFR § 4.14. To receive both ratings, your file must demonstrate that:
- A sleep study confirmed a diagnosis of sleep apnea
- A separate mental health evaluation or psychologist’s report diagnosed insomnia disorder
- Each condition causes distinct symptoms (for example, sleep apnea may cause oxygen desaturation and morning headaches, while insomnia causes difficulty falling asleep and cognitive fatigue)
- Both contribute to different areas of functional impairment, such as concentration loss (mental) versus respiratory limitation (physical)
When documented properly, the VA may assign a combined rating for both conditions using the Combined Ratings Table.
Proving the Connection Between Sleep Apnea and Insomnia
Untreated sleep apnea often worsens insomnia symptoms. Frequent breathing interruptions cause the brain to associate sleep with stress or suffocation, making veterans anxious at bedtime. Over time, this leads to “psychophysiological insomnia” difficulty falling asleep even when the apnea is controlled. In these cases, a medical professional should clarify in writing that insomnia exists independently of apnea, or that apnea has aggravated the insomnia. Under 38 CFR § 3.310(b), aggravation by a service-connected disability still qualifies for compensation.
If your apnea was service-connected first, and your provider confirms that sleep fragmentation and oxygen disruption have caused chronic insomnia, you can file insomnia as a secondary condition. Supporting evidence should include:
- A sleep study report showing ongoing arousals or hypopneas
- Progress notes documenting fatigue or difficulty initiating sleep despite CPAP use
- A nexus letter from a sleep specialist linking apnea to chronic insomnia
- Statements from a spouse or roommate describing restless sleep or snoring-related awakenings
Example: A veteran with service-connected sleep apnea reports persistent sleeplessness even with CPAP therapy. Their VA sleep specialist diagnoses comorbid insomnia and states it is “at least as likely as not caused by chronic sleep fragmentation from apnea.” Because the insomnia contributes to additional cognitive and emotional impairment, the veteran receives a separate 30% mental health rating, combined with their 50% sleep apnea rating.
If your sleep study is negative for apnea but you still experience severe insomnia, make sure your provider clearly records that distinction. The absence of apnea helps confirm that your sleep impairment is not a physical airway issue but rather a psychological or neurological condition. VA raters will then apply the mental disorders criteria (Diagnostic Code 9413 or 9434) instead of DC 6847.
VA attorney tip: During your C&P exam, emphasize symptoms that differ from apnea, like lying awake for hours, difficulty calming your mind, or anxiety around sleep. This prevents the VA from misclassifying your disorder.
How to Win Your Insomnia VA Claim
Winning a VA claim for insomnia requires credible medical evidence, consistent documentation, and a clear link between your symptoms and service. VA adjudicators rely heavily on medical records and functional impact statements when deciding whether to grant compensation, so veterans must build a strong case from multiple sources.
To succeed, you must show that insomnia has diagnostic clarity, a verified connection to service, and functional consequences that limit your work or social life. The VA focuses on whether your insomnia is diagnosed, service-related, and severe enough to interfere with daily functioning. Strong claims typically include:
- Records from a VA or private clinician diagnosing chronic insomnia or noting “persistent sleep disturbance.” You don’t need a sleep study for insomnia, clinical documentation is sufficient. If you also have sleep apnea, clarify that your insomnia symptoms persist even when apnea is treated with CPAP, showing that insomnia is a distinct disorder.
- Deployment or medical records showing high operational tempo, combat exposure, or hazardous duty that disrupted sleep. Duty rosters showing night shifts or guard rotations can also demonstrate how service interfered with normal sleep cycles.
- A statement from a medical professional explaining that it is “at least as likely as not (50% or greater probability)” your insomnia began in service or was worsened by a service-connected disability. This nexus letter must include a clear rationale referencing your medical history and known effects of stress, pain, or trauma on sleep.
- Other supporting documentation such as treatment notes and prescription records for sleep medications.
- Written accounts from family, coworkers, or fellow service members describing your sleep struggles, fatigue, or changes in behavior. VA accepts credible lay testimony as competent evidence of observable symptoms.
By establishing a solid chain of evidence from service exposure to medical diagnosis and functional limitation, you strengthen your case for a compensable insomnia rating and avoid common denial reasons such as “no nexus” or “no functional impairment.”
How to Win Your VA Claim
Having trouble with VA’s complicated procedures? We can help!
Get our FREE ebook The Road to VA Compensation Benefits.
Documenting the Functional Impact of Insomnia
VA ratings are based on functional impairment, not just symptoms. Chronic insomnia alone doesn’t guarantee compensation unless it demonstrably limits your ability to function. A veteran who regularly sleeps only three hours per night and misses work due to exhaustion provides stronger evidence than one who reports occasional sleeplessness. Common functional effects that strengthen a claim include:
- Reduced work performance due to fatigue or difficulty concentrating
- Irritability or social withdrawal impacting family relationships
- Cognitive lapses such as forgetfulness or poor decision-making
- Depressed mood or anxiety directly resulting from long-term sleep loss
Veterans must provide evidence showing how sleep loss affects everyday activities, work performance, and social interaction. This helps raters determine whether symptoms cause mild, moderate, or severe occupational and social impairment, ensuring the correct percentage is assigned. Examples of supporting evidence:
- Sleep logs or diaries tracking total sleep time, awakenings, and fatigue
- Provider statements or functional‑impact questionnaires describing limitations in attention, reliability, or mood
- Lay statements from family, roommates, or supervisors describing visible exhaustion, irritability, or forgetfulness
- Employment records showing absenteeism, errors, or disciplinary actions tied to fatigue
The C&P Exam for Insomnia
The Compensation and Pension (C&P) exam is one of the most important steps in any VA disability claim for insomnia. This evaluation helps the VA determine whether your condition is service-connected and how severe your symptoms are. For many veterans, the C&P exam is the make-or-break moment in the claims process. During the C&P exam, a licensed clinician (usually a psychologist, psychiatrist, or nurse practitioner) will:
- Confirm that you have a current diagnosis of insomnia or a related sleep disorder.
- Assess the functional impact of your symptoms on work, relationships, and daily life.
- Provide a nexus opinion, explaining whether your insomnia is “at least as likely as not” caused by or aggravated by service or another service-connected condition
Before the appointment, the examiner reviews your C-File (claims file), which contains your service treatment records, prior C&P exams, medical history, and lay statements. They use this information to form their medical opinion under 38 CFR § 4.1–§ 4.10, which requires an understanding of how the condition affects “ordinary conditions of daily life, including employment”. During the exam, expect questions about:
- Sleep patterns: How long it takes you to fall asleep, how often you wake up, and how many total hours you get each night.
- Daytime functioning: Whether you feel fatigued, irritable, or struggle to concentrate.
- Onset and history: When you first noticed sleep problems and whether they began during or after service.
- Mental health or physical links: If you have PTSD, chronic pain, tinnitus, or another rated condition that affects sleep.
- Medication and treatment: Whether you’ve tried cognitive behavioral therapy (CBT-I), prescription sleep aids, or other interventions.
- Each answer helps the examiner assess whether your condition meets the VA’s diagnostic and rating criteria for mental health conditions, including chronic sleep impairment
The examiner evaluates severity based on how insomnia affects your daily functioning. Even if you have medical documentation of sleep difficulty, the VA will not assign a compensable rating unless the evidence shows occupational or social impairment. The C&P report may include phrases such as:
- “Symptoms cause occasional decrease in work efficiency” → Typically supports a 30% rating
- “Symptoms cause reduced reliability and productivity” → Supports a 50% rating
- “Symptoms cause deficiencies in most areas ” → Supports a 70% rating
- “Symptoms cause total impairment” → Supports a 100% rating
This functional assessment is crucial because it directly determines your insomnia VA rating. To make the most of your C&P exam, bring documentation that reinforces your claim. The goal is to provide objective proof that your insomnia is chronic, service-related, and functionally limiting. Bring copies of:
- Recent medical records from VA or private doctors showing an ongoing insomnia diagnosis.
- Sleep logs or diaries documenting poor sleep patterns over time.
- Medication records showing long-term use of sleep aids or sedatives.
- Statements from family or coworkers describing daytime fatigue or mood changes.
- Nexus letters or mental health notes linking insomnia to service or a rated condition.
You can also bring your own notes outlining how your sleep problems affect your work performance or family life. These real-world details often strengthen the credibility of your account. During a C&P exam for insomnia, the examiner will evaluate:
1. Insomnia Symptoms
- Difficulty falling or staying asleep
- Early morning awakening
- Daytime fatigue, cognitive impairment, irritability, etc.
2. Medical History
- Onset of sleep issues (during service or after)
- Any documented complaints in your service records
- Relationship to other conditions (e.g., PTSD, depression)
3. Functional Impairment
- Impact on work, daily tasks, concentration, mood
- Whether symptoms affect your ability to secure or maintain employment
If you believe the examiner ignored your medical records, dismissed your lay statements, or failed to consider secondary causes, your representative can challenge the adequacy of the exam.
Under 38 CFR § 4.2, an examination is inadequate if it lacks supporting rationale or doesn’t address all relevant medical evidence. In those cases, you can request a new exam or an independent medical opinion (IMO). Veterans often succeed on appeal when they highlight deficiencies in the original report, such as:
- The examiner didn’t review the full C-File.
- The report lacked explanation for ruling out service connection
- The examiner mischaracterized insomnia as a “temporary sleep issue”
- The rationale didn’t address secondary aggravation (e.g., insomnia caused by PTSD or chronic pain)
By identifying these errors early, you can ensure that the VA considers a complete and accurate medical opinion during your claim review.
A well-documented C&P exam is the foundation of a successful insomnia claim. Veterans who attend prepared with records, consistent descriptions, and clear examples of daily impairment are far more likely to receive a favorable rating.
Be detailed but truthful, focus on function over frustration, and remember: even if the initial exam is unfavorable, VA regulations allow you to challenge its adequacy and submit new evidence to correct the record.
Tips to Prepare for Your C&P Exam for Insomnia
The C&P exam is one of the most critical parts of your claim. Even when medical records show a diagnosis, many insomnia claims are denied because veterans under-report symptoms or fail to link their sleep problems to service. Proper preparation helps ensure that the examiner fully understands how insomnia affects your life and meets the requirements for a compensable rating.
Before your appointment, review your VA C-File or electronic health record. Look for inconsistencies that might confuse the examiner, such as missing treatment dates or notes implying your sleep issues are “temporary.” If you find any errors, bring supporting documents like private medical records or deployment health assessments that clarify your history. Accuracy is key; examiners rely heavily on this file when forming opinions.
Describe your sleep problems in specific, measurable terms. Avoid vague statements like “I can’t sleep.” Instead, explain how insomnia looks in your day-to-day life:
- How many hours you actually sleep each night
- How long it takes you to fall asleep
- How often you wake up and why (pain, nightmares, anxiety, noise)
- How you feel the next day—exhausted, forgetful, irritable, or unable to focus
If your sleep problems began in service or worsened afterward, clearly describe the timeline. Example: “My insomnia started during my deployment to Kuwait in 2006 and never improved, even after returning home.” These concrete details help the examiner assess severity, frequency, and duration, which are the three main factors VA uses to determine disability ratings.
VA ratings are based on how much a condition interferes with work, relationships, and daily life, not just whether it exists. During the exam, give examples of how lack of sleep affects your ability to function:
- Missed workdays or reduced reliability due to exhaustion
- Poor concentration or errors on the job
- Strained relationships from irritability or mood swings
- Avoiding social interaction because of fatigue
These real-world examples transform your claim from “I can’t sleep” into documented functional impairment, which is what the VA compensates. Bring copies (or at least a list) of documents that support your statements. The examiner may not have all your most recent records in their system. Examples include:
- Recent medical or therapy notes showing ongoing treatment for insomnia
- Medication history showing long-term use of sedatives, antidepressants, or sleep aids
- Sleep logs or journals tracking nightly hours, awakenings, and fatigue
- Lay statements from your spouse, roommate, or coworkers describing your sleep struggles or daytime symptoms
Physical evidence prevents the VA from downplaying your condition as “occasional” or “mild”. If your insomnia stems from another service-connected disability (such as PTSD, chronic pain, or tinnitus) make sure the examiner knows this. Say plainly, “My insomnia got worse after my back injury,” or “Nightmares from PTSD keep me awake.” This helps the examiner document the relationship properly, which is crucial if you’re seeking a secondary service connection.
Veterans often minimize their struggles out of habit or pride. Unfortunately, the VA takes your words literally. If you say “I get by fine,” the examiner may record that you’re not significantly impaired, even if you’re barely functioning. Be truthful and specific. You’re not complaining… you’re documenting.
If the examiner uses clinical terms, you’re unfamiliar with, like “sleep latency,” “sleep architecture,” or “secondary gain”, don’t guess. Ask them to rephrase. Answering incorrectly or hesitating can lead to misunderstandings in the report.
Write down what was asked and how long the appointment lasted. This helps if you later need to challenge an inadequate exam (for instance, one that was rushed or ignored key issues). Once the results are available, review your C&P report through My HealtheVet or request a copy through your VA regional office. If the examiner omitted details, contradicted medical evidence, or provided no rationale, those are valid grounds for appeal.
Think of the C&P exam as your one chance to explain the full story of how insomnia affects your life. Honesty, preparation, and clear examples of daily impact can make the difference between a denied claim and a properly rated award. The more credible and consistent your statements are, the easier it is for the VA to apply the correct percentage under the General Rating Formula for Mental Disorders.
Proving a 50% Insomnia Rating
To earn a 50% VA disability rating for insomnia, you must show that your condition causes “reduced reliability and productivity” in daily life or employment due to sleep-related symptoms. Under 38 CFR § 4.130, this rating reflects a moderate-to-severe impact on occupational and social functioning; more than occasional inefficiency, but not complete incapacity.
At this level, the VA looks for evidence that chronic sleep impairment leads to ongoing emotional, cognitive, or behavioral issues such as fatigue, poor focus, irritability, or reduced motivation. The 50% criteria can apply whether insomnia is rated as a stand-alone mental disorder or secondary to another service-connected condition like PTSD, anxiety, or depression.
To qualify for a 50% rating, documentation must show a pattern of consistent impairment, not just occasional sleeplessness. The VA examines:
- Frequency and duration: Nightly sleep limited to three to four hours, with multiple awakenings
- Functional limitations: Reduced concentration, missed work, and strained social relationships
- Medical treatment: Use of prescription sleep aids, therapy, or ongoing psychiatric care
- Occupational reliability: Performance evaluations or lay statements confirming decreased productivity
The VA’s mental health rating schedule defines this tier as “occupational and social impairment with reduced reliability and productivity”, which can result from:
- Flattened affect or lack of emotional responsiveness
- Difficulty understanding complex tasks due to fatigue
- Impaired memory or judgment
- Disturbances of motivation and mood
- Difficulty maintaining work or social relationships
Example: A 37-year-old veteran with a service-connected generalized anxiety disorder (30%) reports severe insomnia that began during deployment in Iraq. Despite therapy and medication, he averages only three hours of sleep per night and struggles with concentration and irritability.
- Work impact: His supervisor documents frequent mistakes and absences due to exhaustion
- Medical evidence: His psychiatrist notes chronic insomnia secondary to anxiety and documents increased anxiety levels tied to sleep deprivation
- Lay statements: His spouse confirms that he wakes multiple times a night, often due to tension or racing thoughts
- C&P findings: The examiner reports “reduced reliability and productivity due to chronic sleep impairment and anxiety”
Based on this evidence, the VA raises his overall mental health rating from 30% to 50%, acknowledging that insomnia significantly worsens his ability to function at work and at home.
Get Help With Your VA Disability Claim
Supporting Evidence for the 50% Claim
When seeking a 50% rating for insomnia, the strength of your claim depends almost entirely on documentation. VA raters must see consistent, verifiable evidence that your insomnia causes reduced reliability and productivity in daily life and employment. Without that proof, the VA may assign a lower rating, even if your symptoms are severe. The following evidence types are most effective when combined in a single, cohesive record:
- C&P exam report noting reduced reliability and productivity: The most persuasive evidence for a 50% insomnia rating comes directly from the VA’s Compensation & Pension (C&P) examination. The examiner’s description of “reduced reliability and productivity” due to chronic fatigue, concentration problems, or mood changes is what often moves a claim from 30% to 50%. When an examiner explicitly notes that sleep deprivation interferes with work performance, task completion, or emotional stability, that language directly satisfies the regulatory criteria in 38 CFR § 4.130. Veterans should ensure their exam captures not only sleep loss but also how it manifests in their daily life…missed deadlines, irritability with coworkers, or difficulty maintaining focus.
- Mental health treatment records showing insomnia with functional impact: Ongoing mental health treatment records serve as vital evidence that insomnia is chronic and impairing, not occasional or situational. Progress notes from psychiatrists, psychologists, or counselors documenting poor concentration, low motivation, and persistent fatigue can show that the condition affects more than just sleep; it disrupts overall functioning. Consistent documentation over time proves both continuity and severity, two major factors VA adjudicators rely on when assigning ratings. The use of prescribed sleep medications or cognitive behavioral therapy for insomnia (CBT-I) should also be included, as it supports the argument that your condition requires continuous treatment.
- Nexus letter linking insomnia to service or SC condition: A medical nexus opinion is essential for establishing connection. The letter should clearly state that your insomnia is “at least as likely as not (≥50% probability)” related to your service or to an existing service-connected disability such as PTSD, chronic pain, or tinnitus. Strong nexus statements include a brief explanation of how military factors, like combat stress, environmental exposures, or pain, physiologically and psychologically contribute to insomnia. For example, a psychologist might cite deployment-related hyperarousal or the impact of chronic musculoskeletal pain on sleep maintenance. A clear, well-rationalized nexus letter is often what distinguishes an approved claim from a denial under 38 CFR § 3.102 and § 3.310.
- Lay statements (from you, coworkers, family) showing how insomnia affects your life: Lay evidence plays an important role in bridging the gap between medical findings and lived experience. Statements from family members, roommates, or supervisors can help illustrate how insomnia affects your ability to function day to day. Examples might include descriptions of pacing at night, frequent naps during the day, irritability, or mental fatigue at work. According to 38 CFR § 3.159(a)(2), such testimony is considered competent when it involves observable symptoms. These statements help VA adjudicators visualize how the condition impacts your social and occupational reliability and are key elements of a 50% rating. The most effective lay statements include specific, dated examples rather than generalized claims like “they don’t sleep well.”
- Work performance evaluations showing decline due to fatigue: Employment records or performance reviews that note declining productivity, errors, or absences caused by fatigue are particularly persuasive. These documents show the functional loss that VA ratings are meant to compensate for. For example, a veteran whose supervisor reports increased mistakes, irritability, or tardiness due to lack of rest provides tangible proof that insomnia causes occupational impairment consistent with the 50% rating level. For self-employed veterans, customer feedback, missed appointment logs, or even personal business journals may serve a similar function. This evidence demonstrates that insomnia affects your ability to sustain gainful employment, a factor VA considers under both 38 CFR § 4.130 and TDIU eligibility guidelines.
How to Increase a VA Rating for Insomnia
To increase your VA rating for insomnia, you need to demonstrate that your symptoms have worsened and now meet the criteria for a higher rating under the VA’s mental health rating schedule (38 C.F.R. § 4.130). Additionally, untreated insomnia contributes to depression, PTSD, anxiety, cardiovascular disease and other illnesses which may be claimed as secondary conditions.
Determine Your Current Rating and Code
Before you can request a higher rating, it’s important to understand how your insomnia is currently classified. You can find this information in your VA decision letter or by logging into your VA.gov or eBenefits account. Most insomnia claims fall under one of the diagnostic codes for mental health conditions because chronic sleep impairment is rated as a mental disorder symptom under 38 CFR § 4.130. For example, if your insomnia is linked to PTSD, it will likely fall under Diagnostic Code 9411; if it’s associated with depression, it may fall under Code 9434. Understanding which diagnostic code your condition is evaluated under will help you align your medical evidence with the appropriate rating criteria.
Maximize Your Benefits
Unhappy with your VA decision? We’re here to help. Contact us for a free review of your case.
Because insomnia is usually rated as part of a broader psychiatric condition, knowing the primary service-connected diagnosis is critical. If the VA has rated you for PTSD, anxiety, or depression, your insomnia symptoms are typically considered part of that evaluation. However, if insomnia causes distinct occupational or social impairment beyond the primary condition, you can seek an increased or separate rating by demonstrating that the sleep disorder independently limits your functioning. For instance, if you’re already rated 30% for anxiety but your insomnia has worsened to the point where you miss work or isolate socially, you can request reevaluation for a higher rating level under the same code.
Understand the Rating Criteria
VA mental health ratings are based on the degree of functional impairment rather than symptom count alone. The schedule provides six possible levels (0%, 10%, 30%, 50%, 70%, and 100%), each tied to specific language describing how symptoms impact occupational and social performance. To increase your insomnia rating, you must demonstrate that your symptoms now match a higher level of impairment than when you were last rated. For example:
- If you were rated 30% for chronic sleep impairment with occasional work inefficiency, you might now qualify for 50% if fatigue, concentration problems, or mood instability reduce your reliability or productivity
- If you were rated 50%, but now experience near-continuous anxiety, panic, or inability to function independently due to insomnia, you may qualify for 70% or 100% (38 CFR § 4.130)
It’s essential that new evidence shows this measurable worsening: either through medical evaluations, workplace records, or lay testimony.
Appeal Paths
- Request a Higher-Level Review : This involves a senior VA reviewer re-examining the same evidence for errors in judgment or application of law. You cannot submit new evidence under HLR, so this path is best for cases where the VA overlooked or misinterpreted existing records.
- File a Supplemental Claim : If you have new and relevant evidence—such as updated medical records, a nexus letter, or proof of worsened symptoms—you can file a Supplemental Claim under 38 CFR § 3.2501.
- File a Board Appeal : For complex or disputed claims, you may appeal to the Board of Veterans’ Appeals (BVA). This route allows you to choose between a direct review, a hearing, or a submission of new evidence
Selecting the right appeal path depends on whether you need to correct a VA error or provide new documentation showing worsening impairment. Every veteran’s situation is unique, so the best strategy for increasing your rating depends on your specific medical and occupational evidence. If your insomnia is more frequent or disruptive, request an updated evaluation and submit new treatment notes from your physician or therapist.
If you believe the VA failed to consider functional limitations like absenteeism, poor work performance, or strained relationships, include detailed lay statements or employer documentation with your appeal. In cases where insomnia has made full-time employment impossible, you may also qualify for Total Disability based on Individual Unemployability (TDIU), which pays at the 100% rate even if your combined rating is lower.
The key to success is providing new, credible, and detailed evidence showing that your symptoms have worsened since your last evaluation. VA law requires that increased ratings be based on current severity, not past assessments, so keeping your medical documentation updated is the surest way to achieve a higher rating.
Insomnia and Secondary Conditions
Even when the VA assigns a low rating for insomnia, veterans can often increase their total compensation by identifying and claiming secondary conditions caused or aggravated by chronic sleep loss. Under 38 CFR § 3.310(b), a secondary condition is any new disability that results from or is worsened by an existing service-connected disorder. This regulation allows veterans to “stack” related conditions, each with its own rating, to increase their combined percentage or potentially qualify for Total Disability based on Individual Unemployability (TDIU).
What Conditions Are Secondary to Insomnia?
- Chronic Fatigue Syndrome: Prolonged sleep deprivation can lead to symptoms that mimic or contribute to CFS (persistent exhaustion, memory lapses, and post-exertional malaise). If you’ve been diagnosed with CFS by a VA or private physician, documentation should show that fatigue patterns directly stem from insomnia rather than another medical cause. A physician’s nexus letter should explain how the long-term sleep disruption and immune system dysregulation caused by insomnia contributed to your fatigue diagnosis
- Headaches and Migraines: Sleep deprivation is a well-documented trigger for both tension headaches and migraines. Insomnia alters neurotransmitter balance and increases muscle tension, which can lead to recurrent head pain. A neurologist or primary care provider can support this link by noting in medical records or a nexus letter that headache frequency and intensity increased due to sleep loss. Maintaining a headache diary alongside your sleep log can further demonstrate the cause-and-effect relationship.
- Cognitive Impairment: Insomnia affects short-term memory, attention, and executive functioning. Neuropsychological testing can document measurable decline in these areas, providing strong evidence of functional impairment. If cognitive issues developed after or worsened with your insomnia, a provider should note that chronic sleep deprivation contributes to cognitive dysfunction, distinguishing it from unrelated neurological disorders. These findings also reinforce higher mental health ratings since the VA’s evaluation formula considers cognitive impact under 38 CFR § 4.130.
- GERD (Acid Reflux): Poor sleep can increase stomach acid production and delay gastric emptying, worsening reflux symptoms. Veterans often report nighttime heartburn or regurgitation that interrupts sleep. To connect GERD secondarily to insomnia, a gastroenterologist or primary care provider must explain that stress and hormonal changes from chronic insomnia exacerbate reflux beyond its natural course. Supporting evidence includes endoscopy reports, medication records, or statements documenting worsened symptoms on nights with poor sleep.
- Hypertension (High Blood Pressure): Medical studies consistently show that chronic insomnia increases the risk of cardiovascular dysregulation and sustained hypertension. The body’s stress response raises cortisol and adrenaline, keeping blood pressure elevated even during rest. A physician can provide a nexus opinion stating that insomnia likely contributed to or aggravated your high blood pressure. Including blood pressure logs and medical literature citations in your file strengthens the secondary claim
- Tinnitus (Aggravation): Sleep deprivation intensifies how the brain perceives tinnitus, making the ringing or buzzing seem louder and more intrusive. Many veterans report that insomnia makes tinnitus harder to ignore, increasing anxiety and distress. An audiologist or ENT should state in writing that the veteran’s insomnia exacerbates tinnitus perception and affects overall functional ability. This distinction allows the VA to recognize tinnitus aggravation as a valid secondary factor under 38 CFR § 3.310(b).
- Diabetes (Aggravation): Chronic insomnia disrupts insulin regulation and increases stress hormone levels, which can worsen blood sugar control. If you already have service-connected diabetes, your provider can write a nexus letter explaining that poor sleep has aggravated your condition. Documentation showing higher A1C readings or medication adjustments after the onset of insomnia helps establish causation.
Total Disability Individual Unemployability (TDIU)
For veterans whose insomnia and related conditions make it impossible to maintain full-time employment, Total Disability based on Individual Unemployability (TDIU) may provide compensation at the 100% rate, even when the combined rating is below 100%.
Chronic sleep deprivation can severely limit focus, productivity, and emotional stability, especially when paired with other service-connected conditions like PTSD, pain, or depression. If your insomnia symptoms prevent you from holding a steady job or performing essential occupational tasks, you may qualify for TDIU consideration under 38 CFR § 4.16. Get a free evaluation of your case here.
Frequently Asked Questions
The VA does not use a specific laboratory test to diagnose insomnia. Instead, it relies on your C&P exam, service and medical records, and any supporting documentation, such as sleep logs or mental health evaluations. The examiner confirms whether insomnia meets diagnostic criteria and determines its connection to service or a rated condition. If another sleep disorder like apnea is suspected, the VA may order a sleep study, but insomnia itself is a clinical diagnosis based on your reported symptoms and functional impairment.
Insomnia is less about a specific number of hours and more about persistent difficulty falling or staying asleep. Clinically, regularly sleeping less than six hours per night or waking up multiple times with fatigue during the day meets the threshold for insomnia disorder. The VA looks at duration, severity, and impact not just sleep quantity.
The most common service connections for insomnia are PTSD, chronic pain, and tinnitus. Research indicates that up to 90% of veterans with PTSD experienced sleep disturbances and disorders, making PTSD the leading secondary cause of insomnia claims. Pain-related insomnia is also common among veterans with orthopedic or nerve injuries that prevent restful sleep.
You’ll need a medical diagnosis, documentation of in-service occurrence or aggravation, and a medical nexus linking the condition to service. The VA also requires evidence showing functional impact, like missed work, decreased productivity, or social withdrawal. Together, these elements satisfy the criteria under 38 CFR § 3.303 for direct service connection or § 3.310 for secondary connection.
If you’re rated for insomnia alone, typically between 0% and 30%, consider whether your symptoms are part of a broader mental health condition such as anxiety, depression, or PTSD. Insomnia is often a component of another service-connected disorder, and combining those claims can yield a higher overall rating. Veterans can request a mental health evaluation to explore this connection and potentially receive a reassessment under the broader General Rating Formula for Mental Disorders.
If denied, review your VA decision letter to identify what was missing: most denials occur because of a lack of nexus or insufficient evidence of daily impairment. You can file an appeal within one year through a Higher-Level Review, Supplemental Claim, or Board Appeal, depending on whether you have new evidence or believe the VA made an error. Adding a strong nexus letter or updated treatment notes often turns a denial into an approval on review.